Long-term care system in crisis
Posted: May 30, 2018
(May 30, 2018)
By: Doug Diaczuk, Thunder Bay News
THUNDER BAY – When Mariann Jollineau had to move her father into long-term care, the experience was stressful and challenging for the entire family. She is grateful to have found a home for him and for the dedication of those responsible for his care, but regular shortages in staff continue to cause concern about the quality of care her father is receiving – a situation all too common for many families across the province.
“When there are shortages, sometimes there is one personal support worker and one registered practical nurse on a floor of 32,” she said. “That’s nuts. No one would allow that in prison, no one would allow that in a daycare, but it happens where we are and that’s not right.”
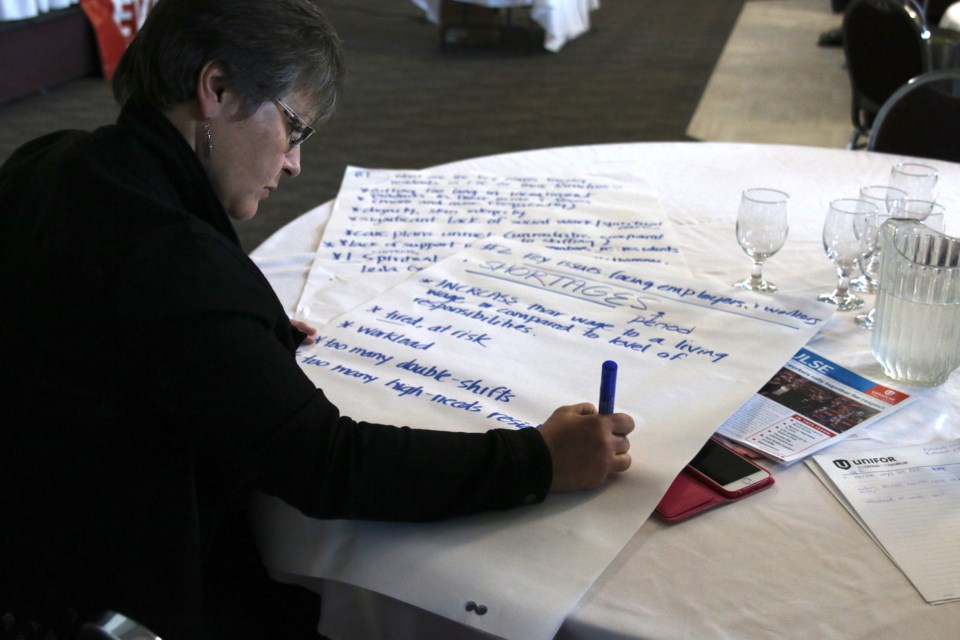
Jollineau was one of several to voice concerns during a town hall meeting on Tuesday hosted by Unifor Local 229 on what it is calling the long-term care crisis.
There are six long-term care facilities in the city of Thunder Bay and Unifor represents more than 2,500 workers in the field. According to Keri Jefford, Unifor Local 229 president, there remains a chronic shortage of PSWs in local facilities, which is due in part to no legislation under the Long-Term Care Act that requires a minimum staffing level or minimum hours of care.
“Some of the issues is legislation changes to make employers and owners of for-profit and private clinics have basic minimum staffing levels and funding also needs to increase and workers need more time with the residents,” she said.
Natalie Mehra, executive director of the Ontario Health Coalition, spoke during the meeting and she said staffing shortages is an issue impacting long-term care homes across the province.
“You have a critical shortage of staff here and that continues to be a major problem that needs to be addressed,” she said.
“Bottom line, even where there are staff shortages in the community, homes are working short staffed because there is no regulated level of care in long term-care homes and it has to be made a priority in the administration that they have to have enough staff,” Mehra continued. “It has to be a political priority of government that they have to provide enough staff.”
During the town hall meeting, several solutions were offered by staff at long-term care homes in the city and family members of residents, which included not opening anymore for-profit or private homes, increase the worker to patient ratio, and wage increases to incentivize more people into the profession.
“This really helps to illuminate what the solutions are,” Mehra said. “A long-term care home itself cannot solve the staffing crisis you have in Thunder Bay. That takes political leadership, resources, and planning to ensure the care bodies moves to where the care is needed and there are incentives to do that.”
Solutions needed now
Staff shortages in long-term care homes are detrimental to not only residents, who may experience a reduced quality of care, but also creates added pressure on staff, which can lead to burn-out and deter others from entering the field.
“The quality of care now is less than it was two years ago, 10 years, 15 years ago,” Jefford said. “The types of residents in long-term care now, more than 90 per cent of them are dealing with dementia issues, there are complex health issues.”
Staff is also forced to provide care for more and more patients in a much shorter time period. In some homes, staff have only six minutes to prepare residents in the morning and Unifor is challenging anyone to run through a morning routine in under six minutes.
“That really starts to wear down on the people providing the care because they do enter this field because they want to care for the residents and want to do the very best for them and most of them are leaving their shift feeling they haven’t met the basic needs of their residents,” Jefford said.
“Already the ball is moving down the field, we just have a little further to go to actually get some real concrete commitments and make them happen once the election is over,” she said.
Jollineau and several other local families have sent a letter to the Ministry of Health and met with management at Hogarth Riverview Manor to discuss how to provide their family members with the best quality of care.
“No one party is responsible, it’s all of our responsibility to be aware and find out,” she said. “You really don’t know until you are in there, until your loved one needs something and it’s not happening and their care starts to decline more than you expect it to.”
And it is not the fault of the staff, Jollineau said, calling their work excellent. She recognizes those who enter the field do so because they want to help others live with respect and dignity and provide the best quality of care they can. But it cannot be done alone. They need a little help, just like those they work so hard to care for.
“When the staffing is right, it’s beautiful, they are not stressed out, they engage, they are there because they want to be there,” Jollineau said. “You feel for them when they are stressed because you know it transfers over to the care they are able to give. It’s a win-win if we can increase it effectively. I just think it takes more creative thinking.”