RELEASE & REPORT: A Call to Conscience: New Report on the COVID-19 Crisis in Long-Term Care in Wave 2 Reveals Huge Gaps in Ford Government’s Response
Posted: December 17, 2020
(December 17, 2020)
Click here for printable version of media release
Media Release
Coalition Calls for Urgent Improvements as Staffing and Care is Collapsing & Large Outbreaks Spread
Toronto – In the last 24 hours alone 18 residents have died and there have been 115 new reported COVID-19 infections in Ontario’s long-term care homes.
The second wave of COVID-19 hit long-term care on August 30 with the outbreak at Extendicare’s West End Villa in Ottawa. Over the following weeks, that outbreak grew and outbreaks spread across the city. By the end of the month, long-term care homes across the province were falling into outbreak, first into the hotspots, then from border to border across the south, into Simcoe Muskoka and up to Thunder Bay.
As of December 15, four-thousand five hundred and ninety-four residents and staff had been infected in the second wave (since September 1). Including yesterday’s death toll, the number of residents that have died in the second wave alone is more than 700.
Clearly the measures taken in and after Wave 1 were not sufficient, says the Ontario Health Coalition.
A new report released today by the Ontario Health Coalition does a deep dive into the policies and plans by the Ford government and reveals what has gone wrong.
“There has been a failure of leadership in this province and a failure to competently plan for the second wave. We are now paying the price in the most horrible of ways,” said Natalie Mehra, executive director of the Ontario Health Coalition and author of the 66-page report titled A Call to Conscience: The COVID-19 Crisis in Ontario’s Long-Term Care Homes.
“The most egregious failure by the Ford government is their total refusal to recruit the thousands of staff needed to replace those who are sick and who have left. Without staff there is no care and infection control,” she said, citing homes where, right now, ten months into the pandemic, segregating COVID-positive residents from those who are not infected has either not happened or has fallen apart because there are no staff to do it.
“The second major omission is the provincial government’s refusal to hold the homes accountable for failure to provide PPE and needed supplies, ensure that infection control practices are actually being done, and have enough staff to give residents care and keep them safe,” she said. Most of the homes are for-profit and they have close ties to this government. “The government made a priority of passing a home care privatization act and a bill to indemnify the long-term care home owners from liability instead of staffing up the homes for the second wave, building testing and contact tracing capacity for when schools opened, and planning systematic responses early on when outbreaks can be stopped. There has been a complete failure in planning and an unconscionable failure in accountability.”
The report evaluates the tangled web of directives, guidance, policies that the Ford government and Public Health Ontario leaders have created and finds gaping holes, reports the Coalition. Among the key findings:
- Improvements have been made in stopping staff from working in multiple homes, but agency staff (temps) are expressly excluded and as staffing has collapsed in home after home, they are using more agency staff than ever. Wages have not been improved, except for temporary pandemic pay which has not actually been given to the majority of staff this fall and which is less now than it was in the summer. The government has not required homes to provide full-time work, instead allowing them to replace trained staff with untrained staff and volunteers. In the case of RNs, it has removed the requirement in the Long-Term Care Homes Act that each home have at least one RN on staff 24/7.
- Other improvements include the end of 4-bed shared rooms, which is being done by attrition and is not complete (home operators have not objected as they are paid whether or the beds are occupied or not under changes made by the government).
- There has been a partial improvement as staff have more access to PPE, but the loophole is that PPE only have to be given at staff’s request. Proper supply and use of PPE is not an enforced and accountable and the Coalition cites evidence from a number of homes in large outbreak that have not provided their staff with PPE including N95 masks, gowns, gloves, disinfectant wipes and other supplies.
- Emergency interventions such as Rapid Response Teams from hospitals (SWAT teams), military intervention, management takeovers have saved lives but they are rare, ad hoc, insufficient and only called in when it is too late. The Coalition reports that in the second wave, up to December 3 only 4 homes had management orders and in most of those, the orders came only after scores of residents and staff were infected. Dozens of homes in large outbreak have no management orders, no management agreements, no teams in to support.
- There have been no fines levied, no licenses revoked, even when the most egregious of neglect and incompetence is evident. In fact, homes with abysmal records have been awarded money from the province for new beds and expansions.
- The failure by the government to build capacity for testing, labs and contact tracing over the summer has been fatal. It contributed to the spread of the virus in the homes through October and November both because test results were slow and because it has resulted in unchecked community spread of the virus this fall. However, home operators also have not cohorted residents showing symptoms.
- The failure to make a plan for systematic response to long-term care outbreaks, early, when they can be stopped, has also been fatal. There still is no systematic intervention, no effective monitoring, little enforcement, no accountability.
- There has been no improvement in quality of management and infection control teams in the homes. In Quebec, the government hired in managers who are paired with infection control specialists for each of their 400 long-term care homes this fall and required them to ensure provincial directives are followed. Ontario has not done anything substantive.
- The most significant problem that is still not addressed is the collapse of long-term care staffing. Without staff, care and infection control cannot happen. Other provinces like British Columbia and Quebec acted months ago to stabilize staffing. Quebec, facing problems similar to Ontario, recruited and trained 10,000 PSWs over the summer and deployed them into the homes in time for the second wave. Ontario’s measures are paltry, piecemeal and unsubstantive.
In home after home, the Coalition reports staffing and care levels crumbling. “This wave is worse than the first, in terms of staffing, because we lost so many staff in the first wave and there is just so little resilience left. As staff get sick there is no one to replace them and home after home falls into chaos,” Ms. Mehra reported.
At the same time, the Coalition reports, there has been extraordinary leadership, particularly on the part of Ontario’s public hospitals, local public health units and EMA. They have held together a system that was facing major cuts and restructuring at the start of the pandemic, and have turned on a dime to build assessment centres, ramp up lab capacity, create field hospitals out of thin air, make the plans and resources that have protected us from a far worse situation. “Measureless self-sacrifice, compassion and care have been exhibited by hundreds of thousands of health care staff at every level,” the report concludes. She notes: On August 31 there was 1 resident and 22 staff infected. On December 15 there were 1,456 currently active (695 residents, 761 staff).
Report
(December 17, 2020)
Click here for printable version of the report found below.
————–
Mission and Mandate
Our primary goal is to protect and improve our public health care system. We work to honour and strengthen the principles of the Canada Health Act. We are led by our shared commitment to core values of equality, democracy, social inclusion and social justice; and by the five principles of the Act: universality; comprehensiveness; portability; accessibility and public administration. We are a non-partisan public interest activist coalition and network.
To this end, we empower the members of our constituent organizations to become actively engaged in the making of public policy on matters related to our public health care system and healthy communities. We seek to provide to member organizations and the broader public ongoing information about our health care system and its programs and services, and to protect our public health system from threats such as cuts, delisting and privatization. Through public education and support for public debate, we contribute to the maintenance and extension of a system of checks and balances that is essential to good decision-making. We are an extremely collaborative organization, actively working with others to share resources and information.
Who We Are
The Ontario Health Coalition is comprised of a Board of Directors, committees of the Board as approved in the Coalition’s annual Action Plan, Local Coalitions, member organizations and individual members. Currently the Ontario Health Coalition represents more than half-a-million Ontarians, 400 member organizations and a network of Local Health Coalitions and individual members. Our members include: seniors’ groups; patients’ organizations; unions; nurses and health professionals’ organizations; physicians and physician organizations that support the public health system; non-profit community agencies; ethnic and cultural organizations; residents’ and family councils; retirees; poverty and equality-seeking groups; women’s organizations, Students for Medicare and other organizations committed to public health care for all under the principles of equity and compassion that underlie the Canada Health Act.
Foreword
The crisis that COVID-19 has presented cast an unflinching light on all of us. Heroic efforts have been made by public health, public servants, public hospitals, and hundreds of thousands of health care workers at every level. True selflessness and self-sacrifice have been demonstrated by so many. Our public health care system and our society have shown extraordinary resilience even after decades of planned undercapacity. Like nothing we have experienced, COVID-19 has brought to the forefront the immeasurable value of public health care in Canada and its foundational principles of equity and compassion. Through the pandemic we have been moved by the countless acts that we have witnessed of care, social solidarity and love by families, communities, local businesses, our health care institutions.
At the same time, COVID-19 has laid bare unconscionable inequities and shortfalls in care for the elderly and other vulnerable people who face discrimination. The suffering of the residents and staff in long-term care has indelibly marked the soul of our province. It is in the memory of those we have lost and in support of those who have experienced the terrible toll of COVID-19 in long-term care that we have written this report. We hope that it will contribute to righting the injustices they have experienced and will result in fundamental reform of and improvements to long-term care in our province.
Table of Contents
Foreword
Introduction
I. Second Wave Vs. First Wave: What Has Changed?
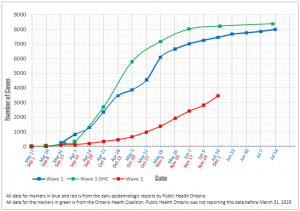
Graph 1. First Wave Compared to Second Wave of COVID-19 in Long-Term Care
II. Factors Contributing To The Spread Of Covid-19 In The First And Second Waves
Table 1: Assessment of Progress in Factors Contributing to the Spread of COVID-19 in Ontario’s Long-Term Care Homes Wave II
a. Improvements & Partial Improvements
Table 2: Management Orders issued & Management Agreements Facilitated
Table 3: Timing of Management Orders/Spread of COVID-19 in Wave II
Table 4. Tracking of Large Long-Term Care Home COVID-19 Outbreaks with no Management Orders/Agreements facilitated by the Ministry of Long-Term Care in Wave II
b. Improvements Followed By Lost Ground
c. Failures
III. Case Studies
-
- Extendicare West End Villa, Ottawa
- Revera Kennedy Lodge, Scarborough
- Extendicare Starwood, Ottawa
- Prescott And Russell Residence, Hawkesbury
Introduction
On August 30, 2020 a second wave of COVID-19 began with the declaration of an outbreak at Extendicare’s West End Villa in Ottawa. The virus quickly spread through that home and across the city. By mid-September eleven Ottawa long-term care homes were in outbreak.[1] By the third week of September, more than 100 residents had contracted COVID-19 in Ottawa’s long-term care homes. At West End Villa alone, in mid-September, sixty-three residents and staff were infected and twenty-four care workers were self-isolating, leaving a perilous staffing shortage in this home that was described in many online reviews as already routinely understaffed even prior to COVID-19.[2] Revelations from the ensuing weeks in long-term care homes with large outbreaks, such as Revera’s Kennedy Lodge in Scarborough and Extendicare’s Starwood in Ottawa and many others since, display horrifying similarities with the conditions exposed at West End Villa in September. Throughout the last three months, the details we have gathered about the current conditions in homes with large outbreaks raise serious questions about why so little had changed in Ontario’s long-term care homes since the first wave of the pandemic.
We are writing this report two months after the devastating revelations about second-wave conditions in Extendicare’s West End Villa and six months after the military report exposing horrific neglect and incompetence in the long-term care homes to which they were deployed. COVID-19 outbreaks in long-term care have now spread from the “hot spots” of Ottawa, Toronto and Peel, first to surrounding regions, and most recently across the south from border to border, and into the north of the province. The number of long-term care outbreaks has increased from 18 to 117, the severity of those outbreaks is increasing, and 3,462 staff and residents have been infected since September 1.[3] The second wave has hit the long-term care sector and the inadequacies in provincial planning and capacity-building have become alarmingly apparent.
In particular, the provincial government made a grave error in failing over the summer in making a coherent capacity-development plan to be ready for the reopening of businesses and schools. Hard-won ground that had been gained in public health measures across the first wave was lost and precious time was wasted. After schools reopened, testing, laboratory and contact tracing capacity was overwhelmed, test backlogs impacted long-term care homes and the community, and unchecked spread of COVID-19 has resulted. The provincial government’s reluctance to put resources and accountability mechanisms in place to improve care levels and staffing, infection control and oversight in long-term care has became undeniable. In fact, a number of the homes have less resilience to successfully defeat a second wave of infections due to loss of vital caregiving staff. Measures such as hospital rapid-response teams, management orders or agreements and help from the Red Cross have been taken in some homes, but these measures remain late, ad hoc and insufficient. Funding has been slow to flow, and desperately needed hospital capacity, including field hospitals or the like, have not been created in time. It has now become evident that provincial policy decisions have not met the stated goal of protecting those most at risk.
How was it possible that six months after the emergency was declared and five months after the government’s action plan for long-term care was released, conditions in a startling number of long-term care homes could be essentially the same as we saw in the first wave? As the outbreaks have expanded through the fall, despite a vast and complex body of regulations, policy, directives and guidance documents, revelations from families and staff showed that many measures have gaps and loopholes expressly written into them. There have been partial improvements to the required measures but vital pieces are missing. For some of the measures, there have been improvements followed by lost ground as a result of the failure to plan and build capacity in the summer. Accountability is still non-existent for homes that do not follow the Infection Protection and Control (IPAC) protections and other measures that are supposed to be in place. There remains no systematic intervention early enough to save lives and provide care in the homes that have outbreaks, and in some there is no evidence of intervention at all. As the fall has progressed and the second wave has gained amplitude, the provincial government made a priority of indemnifying long-term care homes against liability for negligence while at the same time doing substantively nothing to improve staffing and care levels, and accountability and enforcement of protections.
At the same time, it is important to pause to recognize that there have been impressive achievements in capacity building in the midst of crisis. Public Health Units, facing unprecedented restructuring and cuts at the beginning of the pandemic pivoted practically overnight to deploy an army of contact tracers, develop public information, collect data, create assessment centres, produce policies and guidelines and lead a heroic—and too-often unrecognized — effort to get ahead of the virus. Ministry and Public Health Ontario staff have worked doggedly to produce policies to respond to emerging information about the virus. Public hospitals, too, at their own initiative, created assessment centres and field hospitals out of thin air; ramped up laboratory testing capacity; and took on providing vital support – again often unsung – to bolster inadequate infection control, staffing and management in long-term care homes. EMS also leapt in with vital aid in the crisis, filling care needs across the continuum from home care to long-term care and hospitals. Measureless self-sacrifice, compassion and care has been exhibited by hundreds of thousands of health care staff at every level through the pandemic. They have held together a system that has been built on planned undercapacity for decades. They have been redeployed, given up time off, risked themselves and their families, and adapted to ever-changing policies and plans. Their courage, commitment, and what can rightly be described as love, shines.
Since mid-March when the first long-term care outbreaks were reported by local Public Health Units, the Ontario Health Coalition began tracking the spread of the novel coronavirus in long-term care homes and advocating for measures to more effectively contain it. Our Coalition represents more than half-a-million people and more than 400 organizations including care workers and their unions, health professionals, physicians, seniors’ organizations, family councils, residents and patients, and a wide array of community groups who believe in the principles of equity and compassion that are foundational to our public health care system. We have received thousands of phone calls, individual correspondence and social media contacts through the pandemic from residents, patients, workers, health professionals and advocates. We have also conducted two surveys of long-term care staff during the pandemic to gather information about the state of staffing, care and infection control in the homes. These follow a pre-pandemic study we did in partnership with Unifor, in which we consulted more than 350 long-term care home administrators, college PSW program administrators, PSWs, family councils and found total consensus that there was a PSW staffing crisis across the province. We also researched and wrote a major report pre-pandemic on the state of long-term care, looking at acuity, care levels, violence, injury rates, and access to care. This was the latest in a series of reports on the state of this sector that we have released every few years since the turn of the century.
Our Coalition has advocated for reform to improve care in long-term care and across the continuum of care for more than three decades. As such, we have a unique and broad perspective from the front-lines of care about what has happened during the pandemic. We have closely tracked the state of data collection, the approach to treatment and support of residents in long-term care and the policy response to the emergency. We have developed as clear a view as possible on the state of accountability at the level of individual homes, regional public health and health planning governance, and at the provincial level. Our perspective is informed from both the experiences of residents and families, and those of care workers including aides and PSWs, nurses and health professionals, and physicians providing care.
In this report we describe our observations about the spread of COVID-19 in Ontario’s long-term care homes in the first wave and in the second wave to date, analyse the contributing factors and the responses by public health authorities and government, and provide some ideas for measures that are needed urgently.
I. Second Wave Vs. First Wave: What Has Changed?
Current Situation
Though there is no hard and fast date marking the start of the second wave of the COVID-19 pandemic in Ontario, from Public Health Ontario data we can see that case numbers among younger adults began to rise in the late summer. In long-term care throughout the summer months, though outbreaks still began, there were only two that we have found that had more than five cases.[4] The outbreak at Extendicare’s West End Villa was declared on August 30 with one positive case and the numbers expanded from there. Within a few weeks there were eleven long-term care homes in Ottawa with outbreaks, outbreaks began in other regions, and the outbreaks began to spread beyond a few positive cases. Thus, the beginning of September can be described fairly, we believe, as the beginning of the second wave of the COVID-19 pandemic in Ontario’s long-term care homes.
In the last three months both the number and severity of the outbreaks has increased dramatically. At September 1 there were 18 ongoing long-term care outbreaks in Ontario’s long-term care homes.[5] At the time of writing, on December 1 there are 117 currently active outbreaks[6], up from 76 as at October 31.[7] Through October and into November some of the large outbreaks that started in September were resolved — many after terrible loss of health and life — and new large outbreaks started. [Addendum on December 16: By mid-December, in home after home we are seeing a tidal wave of new infections that are spreading with hair-raising speed. These most recent huge outbreaks have happened since this report was written and are not captured in the numbers here.]
Of the currently active 117 Ontario long-term care home outbreaks up to December 1:
- 45 outbreaks include more than 10 residents and staff infected;
- 20 outbreaks include more than 50 residents and staff infected;
- 10 outbreaks include more than 99 residents and staff infected;
- 5 outbreaks include more than 150 residents and staff infected;
- 1 outbreak includes more than 200 residents and staff infected.[8]
According to the province’s epidemiological data for the single day of December 2, there were 707 currently active confirmed cases among long-term care residents and 553 currently active confirmed cases among long-term care staff.[9] By comparison, at the end of August there were there were 3 currently active cases among long-term care residents and 18 currently active cases among long-term care staff.[10]
Looking at the cumulative cases for the second wave to date we can see the sharp escalation in recent weeks:
- The total of long-term care COVID positive cases from September 1– November 24 was 2,826 (2,240 residents, 586 staff).[11]
- The total of long-term care COVID-positive cases from September 1 – December 1 was 3,462 (2,737 residents, 725 staff). [12]
Thus, in the most recent single week, there has been an increase of 636 cases in Ontario’s long-term care homes according to Public Health Ontario’s data.
The Centre for Disease Control in the United States[13] and epidemiologists in Canada[14] have warned that increases in cases among younger people spread to older age groups with a time lag of several weeks. That is what appears to have happened at the beginning of the second wave in Ontario. The significant increase in case numbers among youth and younger adults through September was followed by a sharp increase in case numbers among elderly people a few weeks later.[15] In fact, after trailing the escalations among first the 20 – 39 year-olds then the middle-older age group by a few weeks in the early fall, case numbers among the over-80 age group surpassed all others in mid-October. Current Ontario Public Health epidemiologic data shows that sixty-three percent of Ontario’s COVID-19 deaths are in long-term care[16] and 27 percent of long-term care residents who have contracted COVID-19 in Ontario have died.[17] The current record-high rates of transmission among the general population bode ill for the elderly. Every day lost in establishing effective interventions to stunt the spread of COVID-19 in long-term care risks more suffering and death.
Changes from Wave I
Public Health Ontario was not tracking long-term care outbreaks at the beginning of the first wave of the pandemic. As a result, we began tracking outbreaks and case numbers using local Public Health Unit outbreak reports and following all case numbers in every long-term care home, retirement home and hospital as they were reported by each local Public Health Unit.[18] Throughout the pandemic we have continued to issue reports as frequently as we have the resources to do so, tracking the spread of COVID-19 in long-term care homes and other settings. To find the numbers, we have tracked the outbreak reporting for each outbreak from each local Public Health Unit from beginning to end of outbreak. There are significant differences in the data provided by local Public Health Units and Public Health Ontario’s data. In response to questions about the inaccuracies in Public Health Ontario’s data, and reported problems with their database, the provincial epidemiologic reports began to include numbers from the Ontario Ministry of Long-Term Care database which they contend includes reporting to the Ministry directly from long-term care homes. The data is significantly different between these two central databases and both at times have had significant differences from our tracking, based on local Public Health Units’ reports. Regardless, we are able to plot the trajectory of Wave I and Wave II and get a general sense of the differences.
Using the data from Public Health Ontario and our own data from the first wave, and comparing it to the data reported from Public Health Ontario in the second wave, we can see the trajectory of the first and second waves to date in the graph below. Please note: In mid-April Ontario was processing 2,500 tests per day. By late May, the province was processing between 15,000 and 20,000 tests per day. In November the province was processing 30,000 – 40,000 tests per day. It is not clear the impact of the testing ramp up on the relative shape of the curve in Wave I.
Graph 1. First Wave Compared to Second Wave of COVID-19 in Long-Term Care
Notably, the second wave appears to have started more slowly than the first wave but in the last five weeks (since October 27) the spread of COVID-19 in long-term care has escalated in an alarming way. In the first wave, the most devastating growth in the numbers of staff and residents infected with COVID-19 happened between mid-April and mid-May. In the second wave, it took about 8 weeks for COVID-19 to spread to 1,000 residents and staff (from September 1 to October 27). In that period, the first six weeks (September 1 – October 13) saw approximately 500 cases followed by the second 500 cases in the final two weeks (October 13 – October 27). From October 27 the spread escalated more sharply. Since then we are seeing approximately 1,000 new cases every two weeks.
II. Factors Contributing to the Spread of COVID-19 in the First and Second Waves
Many of the factors contributing to the spread of COVID-19 in Ontario’s long-term care homes that were in evidence in the first wave are still in evidence today. It is no longer the case that we do not understand enough about how the virus is spread. The issue is one of political will. Measures taken to address the factors contributing to the spread of the virus are mostly partial, ad hoc, voluntary and unaccountable. It appears to us that interests and desires of the industry dominate the policy response, even in crisis, despite a wide consensus about the stronger more accountable measures needed from clinical and scientific experts, expert advocates who understand from years of experience the conditions in long-term care homes, unions with tens of thousands of members working in the homes, and thousands of residents and families. Because care and infection control rely on adequate staffing to provide them, the biggest failure by far is the refusal of the provincial government to recruit and train a cadre of staff to get into the homes. We choose the word refusal purposefully. That the Ontario government did not do so in the summer lull is incomprehensible. As the second wave has grown, the continued refusal by our government to take anything other than piecemeal and voluntary measures to improve staffing and care levels is unconscionable. Further, systematic measures for every home that goes into outbreak are still not in place. Many are voluntary. Some are ad hoc or too late. The evidence is clear that even where improvements have been made, they are inadequate to control the large outbreaks that continue to occur in ever increasing numbers and there is no accountability for home operators that fail to implement needed measures.
In Table 1 we have divided the Ontario government’s performance on addressing the factors that are contributing to the spread of COVID-19 in long-term care homes into three streams:
- First, there have been some improvements, for example, the cessation of admitting residents into long-term care homes in outbreak and the end of 4-bed shared rooms, the latter of which is currently happening through attrition and as residents are cohorted. There are other improvements that were partial and still remain inadequate, for example, the increase in PPE supply and improvements to provincial Directive #5 which have changed but are still not adequate to ensure that homes are accountable for actually providing PPE to staff who are exposed to the virus. Emergency interventions such as military teams, hospital rapid response teams and Red Cross support count as improvements though they are limited by being ad hoc, inconsistent, implemented too slowly and often voluntarily, or not implemented at all even when warranted.
- The second set of measures include those in which there were some advances but that ground has been lost after the summer, notably in testing, contact tracing and adequate laboratory capacity. The use of COVID-positive asymptomatic workers is not publicly reported but anecdotally we found that it decreased over the first wave. From direct accounts of staff in homes with large outbreaks in November and December we have found it is in practice again and is being allowed by the province.
- The final group of measures include those that are clear failures. Staffing levels, central to all care and infection control measures, have actually worsened and continue to decline in a number of homes. The failure by the provincial government to set in place a systematic accountable enforced regime to arrest outbreaks early has resulted in fatal consequences. Still today, after months of repeated promises for change, provincial government action to enforce and hold accountable incompetent and negligent operators has been negligible. That thousands of long-term care residents are left in homes even when staffing is perilously low, hundreds or more of them sick with woefully inadequate care as they are dying, is nothing less than barbaric.
Special note: The work of tracing back the orders and policy documents is astoundingly time consuming and difficult. Many documents cross-reference other documents, some of which are out of date or have broken links. These are the vital safety provisions that health system providers such as long-term care homes, retirement homes and hospitals are supposed to follow. There is a dizzying array of Provincial Command Table Memos, Health Coordination Table Memos, Minister’s Orders, Health Minister’s Directives, Long-Term Care Minister’s Directives, other overarching Directives, Guidance, various fact sheets and policy documents, regulations under the emergency act (now moved to the Reopening Ontario (a Flexible Response to COVID-19) Act, and local Public Health Unit documents in addition. There are multiple updates to the various documents and the changes to the provisions are not made clear. The Directives are particularly bad for this. Various iterations of each the Directives are not dated, previous iterations are not reported on the Directives website, and the changes to the provisions in the various new versions are not made clear. Some of them contain different requirements and recommendations. It is a mess, frankly, that needs to be clarified, made consistent and streamlined.
Table 1. Assessment of Progress in Factors Contributing to the Spread of COVID-19 in Ontario’s Long-Term Care Homes Wave II |
| Improvements & Partial Improvements
· Access to PPE, cleaning supplies. Partial improvement, inadequate, at request, not enforced. There are still significant problems for staff accessing a range of PPE and cleaning supplies both in homes in outbreak and homes not in outbreak. · Bar on transfer of patients/residents into long-term care homes in outbreak. Improvement, however there is a loophole. · Bar on 4-bed shared rooms. Improvement, partial as it is in process. · Bar on staff working in multiple long-term care homes. Partial improvement, inadequate, very problematic loophole. · Interventions when outbreaks occur: o Some homes had rapid response teams sent into them and the outbreaks were contained in the following weeks in those homes. Improvement, partial, ad hoc and insufficient. o Some homes had the military sent in and the outbreaks were contained over the following weeks. Improvement, temporary. o Some homes had temporary management orders or agreements and the outbreaks were contained over the following weeks. Improvement, partial, ad hoc and insufficient. |
| Improvements Followed by Lost Ground
· Assessment/testing, contact tracing and laboratory capacity. Improvement over the first wave followed by a total failure to plan for reopening of businesses and schools in the summer leading into the fall, huge backlogs in the fall with devastating consequences. · Asymptomatic staff working. This is allowed under Directive #3 though asymptomatic staff are supposed to work on work isolation. This is not possible for PSWs and nurses in long-term care and no work isolation requirements were ever followed. However, anecdotally, there was improvement in this in Wave I. In Wave II in homes where staffing is collapsing, it is being done more frequently. |
| Failures
· Staffing and care levels. Worse than prior to the pandemic, worse than Wave I. · Quality and accountability of management/ General acountability, enforcement. Nonexistent. There is no accountability for incompetent and negligent management. No plan to address quality problems. · Getting residents the care they need when the long-term care home is in crisis. This is still not happening. · Coordinated, systematic approach. Nonexistent. · Recognition of airborne transmission. This is still not formally recognized in the directives and applied through the measures taken. |
A. Improvements & Partial Improvements
Access to PPE
Directive #5 was amended multiple times to enhance the ability for staff to get access to PPE, including N95 masks. In the most recent version of Directive 5, all staff who are within 2-metres of COVID-positive residents/patients have the ability to obtain an N95 mask upon request. This is an improvement, but it falls far short of a clear requirement for the homes’ management to provide PPE and be responsible for ensuring a high standard for its use. In homes with second wave outbreaks that involve more than 100 residents and staff; care workers have reported that, even as scores of residents and staff were infected, they did not have access to N95 masks or that there are some N95 masks but not in appropriate sizes. In some homes with large outbreaks, we have heard in the preliminary results from our current staff surveys that they do not have access to N95 masks in their sizes and that management is dissuading staff from using N95 masks. Dissuasion techniques include: requiring staff to sign out the masks; training that tells them that the masks are only needed for aerosol-producing procedures; masks are not readily available and it requires a process to search for them; a culture in which staff fear that they will be treated as “a trouble maker” if they ask for PPE or if they complain about staff not using appropriate PPE.
It is not only N95 masks that are lacking. In more than a dozen homes in recent weeks, we have heard from staff who are telling us that the homes are short of gowns and gloves, disinfectant wipes, and a range of supplies are not available when needed. This information was corroborated in our survey of staffing levels in July.
Long-term care home operators should be required to provide appropriate PPE, including N95 masks, gloves, gowns and cleaning supplies and should be responsible for following infection control in accordance with sound IPAC practices and the precautionary principle. They must be held accountable for this.
Bar on transfer of patients/residents into long-term care homes in outbreak
Improvements to Directive #3 on June 10 stopped hospitals from discharging COVID-19 positive patients into long-term care homes and barred long-term care homes from admitting residents when homes are in outbreak.[19] In the first wave, these admissions did happen and likely contributed to the devastating spread of COVID-19 through long-term care homes in the spring, though we have not been able to find any publicly available research that includes backward contact tracing in homes with large outbreaks.
The improvements in this directive have, without question, made a difference. But there is a loophole that, according to advocates, was used last spring and it is not clear whether it is still being used. For both new admissions and readmissions from hospital, under this Directive, local Public Health Unit can allow discharge of patients to homes with COVID-19 outbreaks in agreement with the long-term care home and the hospital.[20] Though consent of the hospital, long-term care home and Public Health are required, applicant consent is not required. The Advocacy Centre for the Elderly had a case that involved this loophole last spring. In the worst possible scenario, as a result of this loophole patients in hospital could be penalized, lose their place on the waiting list, and be subject to exorbitant bed fees for refusing such a transfer. This loophole does not apply to those seeking long-term care placement from the community. It should be removed. No one who is at risk of infection should be transferred into a long-term care home or retirement home in outbreak.
End of 4-bed shared rooms
In the summer one significant improvement began which is still underway: the end of four-bed shared rooms in long-term care homes. On Aug. 28, Ontario issued a new Directive #3 for Long-term Care Homes under the Long-term Care Homes Act. Under the improvements to this directive, both new admissions and re-admissions “from the community or from a hospital (including ALC patients) to a long-term care home or retirement home can occur if: … The resident is placed in a room with no more than one (1) other resident. That is, there shall be no further placement of residents in three or four bed ward rooms.” Directive #3, as updated October 14, still includes this provision.[21]
This change is difficult because it reduces the availability of long-term care spaces in a context of high occupancy and long wait lists but it is necessary and long overdue. It is currently being undertaken by homes as they are cohorting residents and through attrition. Existing 4-bed rooms are being converted to 2-bed rooms as residents are moved out to other spaces while being cohorted, and as residents pass on or leave and new admissions are limited to two people per room. We have not heard of any instances where this directive is not being followed. What we are hearing is that some homes are voluntarily moving residents more quickly to reduce or eliminate 4-bed shared rooms. Funding has been provided to homes to offset their lost funding as a result of this.
Movement of staff between facilities
After a belated recognition that precarious working conditions in long-term care are dangerous, the provincial government made a partial improvement in late April. After April 22 under a regulation under the emergency act, staff who are employees of multiple long-term care homes were required to choose one job.[22] However, there was a very significant loophole expressly written into the regulation. The regulation covers employees of long-term care homes but purposely excludes third-party employees (known as agency staff). Thus, while staff employed by long-term care homes had to choose one home to work in, agency staff continue to be allowed to work in multiple homes. At the same time, long-term care homes were not required to replace lost hours by providing existing staff with full-time work, and, in fact, were expressly allowed by another regulation under the emergency act[23] to replace regular employees and work hours with untrained staff and unpaid volunteers.
As we and many others recommended to the government, while we supported the restriction on working in multiple homes at the same time, this measure could never stand alone. The failure to make concurrent policy to address the knock-on effects of this regulation actually worsened staffing shortages in a significant number of long-term care homes. This, and the actual expansion of the use of agency staff, are among the most significant failures in policy in the pandemic to date (see “Failures” section). Some homes with better wages and hours undoubtedly benefitted by stabilizing their workforce and preventing more entry points for the virus if they voluntarily provided existing staff with full-time jobs and did not contract agency staff who are working concurrently in multiple homes. But for-profit homes with worse wages and scheduling practices replaced PSWs with agency staff and unpaid volunteers. The latter not only continued with woefully inadequate staffing and care levels but can also have even more staff working in multiple homes than prior to the regulation. After much thought, we have named the partial restriction on inter-facility work for long-term care staff as an improvement but with a very serious qualification recognizing that this measure has had contradictory effects, and the negative impacts on workforce capacity, and therefore on care, have been devastating in a number of homes.
Emergency Interventions: Hospital Rapid Response Teams, Military Teams, Management Orders
In response to severe COVID-19 outbreaks in long-term care homes, the Ontario government and public health officials have undertaken a number of crisis measures including the deployment of hospital rapid response teams (colloquially known as SWAT Teams) and military teams, and in rare cases has issued management orders. These are an improvement on doing nothing at all. However, they are only a very partial improvement which has been ad hoc and inconsistent, inadequate, late or not used at all. According to provincial government reporting to December 3, the Ministry of Long-Term Care has:
- Issued 6 Mandatory Management Orders.[24]
[Author’s note: despite the fact that the most recent Government of Ontario Media Release (December 3 as per footnote #23) states that 6 homes had received orders we found a total of 8 management orders announced by that date. This information comes directly from Ontario government press releases. The orders themselves are not posted online. See Table 2 for the list with links to the government media releases announcing the orders.]
- Facilitated 16 voluntary management contracts between Ontario hospitals and long-term care homes.[25]
[Author’s note: We found 14 not 16. Again, these are directly from government and/or hospital media releases. However, there has been a great deal of confusion in government announcements about orders vs. agreements. It appears that the provincial government is counting two of the orders they have issued as agreements.]
- In addition, military teams were sent in to six long-term care homes in the spring/summer.
Management Orders
The Minister of Long-Term Care has had the ability to make management orders for the take over of long-term care homes stretching back years before the pandemic started and arguably could have made those orders earlier in Wave I. The Ontario government passed a regulation under the emergency act in May giving the Ministry more latitude to make management orders in homes with COVID-19 outbreaks.[26] There is little doubt that the homes that were finally given orders after the new regulation was passed in May would have met the threshold (which required non-compliance and reasonable grounds to believe that they could not properly manage the homes) as set out in the Long-Term Care Homes Act (2007). But even after setting a new threshold (the home had to be in outbreak) in May, the Ministry has only used these powers belatedly and only in eight homes. Many homes with terrible outbreaks have not been subject to either management takeover or facilitated management agreements. Most of those that have received management orders were inexplicably late and only happened after scores of residents and staff were infected and deaths were mounting. As such, the new regulation under the emergency act and the use of those powers was an improvement, but in operation it remains too little, too late and inconsistently applied.
Under Ontario’s Long-Term Care Homes Act, all long-term care home owners are required to ensure that the home is a safe and secure environment[27] and the provincial government has an array of powers that enable it to intervene when the Ministry of Long-Term Care has reasonable grounds that the owner cannot manage the home. Specifically, the Ministry has the power to order management takeover or assistance and has the power to revoke the owner’s license to operate the home. There are additional provisions that have passed Third Reading but are awaiting proclamation[28] in the Strengthening Quality and Accountability for Patients Act (2017) that give the Minister additional powers to levy administrative penalties and suspend licenses. There have been confused and inaccurate claims about these powers in media and public statements by government officials. For clarity, we have included the actual provisions here.
Section 156 of the Long-term Care Homes Act states:[29]
(1) The Director may order a licensee to retain, at the licensee’s expense, one or more persons acceptable to the Director to manage or assist in managing the long-term care home. 2007, c. 8, s. 156 (1).
(2) An order may be made under this section if,
(a) the licensee has not complied with a requirement under this Act; and
(b) there are reasonable grounds to believe that the licensee cannot or will not properly manage the long-term care home, or cannot do so without assistance. 2007, c. 8, s. 156 (2).
Section 157 of the Long-Term Care Homes Act states:[30]
(1) The Director may make an order revoking a licence. 2007, c. 8, s. 157 (1).
(2) A licence may be revoked under this section if,
(a) the licensee has not complied with a requirement under this Act;
(b) any person has made a false statement in the application for the licence, or the licensee or any person acting on behalf of the licensee has made a false statement in any report, document or other information required to be furnished under this Act or under any other legislation in relation to the long-term care home;
(c) the conduct of the licensee, a person with a controlling interest in the licensee or, where the licensee is a corporation, the conduct of the officers or directors, affords reasonable grounds to believe,
(i) that the home is not being or will not be operated in accordance with the law and with honesty and integrity,
(ii) that the licensee, officers, directors or persons are not competent to operate a home in a responsible manner in accordance with this Act and the regulations or are not in a position to furnish or provide the required services, or
(iii) that the home is being operated or will be operated in a manner that is prejudicial to the health, safety or welfare of its residents;
(d) a person has acquired control over, or interfered with, the operation of the long-term care home by exercising a security interest contrary to section 107; or
(d.1) a person has acquired control over the operation of the long-term care home by exercising a security interest in accordance with section 107, and the conditions provided for in the regulations apply; or
(e) a person has gained a controlling interest in the licensee without the approval of the Director, contrary to section 109, or a condition of such an approval has been breached. 2007, c. 8, s. 157 (2).
On May 12, 2020 the provincial government issued a new regulation under the emergency act.[31] This new regulation enables the Ministry to make a management order under subsection 156 (1) of the Long-Term Care Homes Act (LTCHA) in an outbreak. The new regulation eliminates the requirements in subsection 156 (2) (a) and (b) of the LTCHA which require that the home both be non-compliant and that there be reasonable grounds to believe the home owner cannot properly manage the home. In Section 2 the Regulation states:
1) The Director is authorized to make an order under subsection 156 (1) of the Long-Term Care Homes Act, 2007 with respect to a long-term care home if at least one resident or staff member in the long-term care home has tested positive for the coronavirus (COVID-19) in a laboratory test.
(2) Subsection (1) applies despite any requirement or grounds set out in the Long-Term Care Homes Act, 2007 or Ontario Regulation 79/10 (General) made under that Act, and despite any other statute, regulation, order or policy.
Thus, the Minister has had longstanding powers to take over the management of long-term care homes and to revoke licenses. Since May 12 the Minister has had even more latitude to do so in long-term care homes with COVID-19 outbreaks. The provincial government has powers, under the amendments to the Long-Term Care Homes Act passed in 2017 to issue fines and suspend licenses. These powers have been underused and the Ministry has not acted to provide needed leadership and accountability in the majority of homes with outbreaks, including the majority of homes with large outbreaks. In fact, any meaningful accountability for negligent and incompetent homes is virtually non-existent.
Table 2: Management Orders issued: |
Management Agreements facilitated: |
| November 25 – Tyndall Nursing Home Mississauga
For-profit. Parent Co. Sharon Village Care Homes Management Order[32] management assumed by Joseph Brant Hospital.
October 27 – Millenium Trail Manor Niagara For-profit. Owned by 955464 Ontario Ltd/ConMed Healthcare Group. Management Order[33] management assumed by the Niagara Health System.
October 9 – Simcoe Manor Home for the Aged Beeton Public. Owned by the Corp. of the County of Simcoe Management Order (initially by Simcoe District Health Unit then by the Ministry of Long-Term Care on October 13)[34] management assumed by Royal Victoria Regional Health Centre.
July 17 – Villa Colombo North York Non-profit home ownership/for-profit management: owned by Villa Colombo Homes for the Aged Inc. and managed by Extendicare.[35] Management Order[36] management assumed by Humber River Regional Hospital
June 4 – Woodbridge Vista Care For-profit. Owned by Sienna Senior Living. Management Order[37] management assumed by William Osler Health Centre.
June 2 – Forest Heights Long-Term Care Kitchener For-profit. Owned by Revera Inc. Management Order[38] management assumed by St. Mary’s General Hospital.
May 25 – Downsview Long Term Care Toronto For-profit. Owned by Gem Health Care Group Ltd. Management Order[39] management assumed by Humber River Regional Hospital.
May 25 – River Glen Haven Nursing Home Sutton For-profit. Owned by Atk Care Inc. Management Order[40] Southlake Regional Health Centre. Extended as a Voluntary Management Agreement August 24.[41]
|
December 3 – Sunnycrest Nursing Home Whitby For-profit. Owned by Sunnycrest Nursing Homes Ltd. Management Agreement[42] management assumed by Lakeridge Health.
December 3 – King City Lodge Nursing Home King City For-profit. Owned by Poranganel Holdings Ltd. Management Agreement[i] management assumed by Southlake Regional Health Centre.
November 28 – Rockcliffe Care Community Scarborough For-profit. Owned by Vigour Ltd./Vigour General Partner Inc. Management Agreement[ii] management assumed by Scarborough Health Network.
November 28 – Langstaff Square Care Community Richmond Hill For-profit. Owned by Sienna Senior Living (2063414 Ont. Ltd.) Management Agreement[iii] management assumed by Mackenzie Health. October 27 – Extendicare Starwood Ottawa For-profit. Owned by Extendicare. Management Agreement[iv] management assumed by The Ottawa Hospital.
September 30 – Norwood Nursing Home Toronto For-profit. Owned by Norwood Nursing Home Ltd. Initially an Order by Toronto Public Health Sept, 30, then a Management Agreement by the Ministry of LTC Oct. 7. [v] Management assumed by Unity Health.
September 25 – Extendicare Laurier Manor Ottawa For-profit. Owned by Extendicare. Management Agreement[vi] management assumed by The Ottawa Hospital.
September 18 – Extendicare West End Villa Ottawa For-profit. Owned by Extendicare. Management Order/Agreement: Initially an Order by Ottawa Public Health Sept. 18, then a Management Agreement by the Ministry of Long-Term Care Sept. 25.[vii] Management assumed by The Ottawa Hospital.
June 15 – Extendicare Guildwood Scarborough For-profit. Owned by Extendicare. Management Agreement[viii] management assumed by the Scarborough Health Network.
June 15 – Hawthorne Place Care Centre North York For-profit. Owned by Responsive Group Inc. Management Agreement[ix] management assumed by North York General Hospital.
June 12 – Orchard Villa Pickering For-profit. Owned by Southbridge Care Homes. Management Agreement[x] management assumed by Lakeridge Health.
June 8 – Altamonte Care Community Scarborough For-profit. Owned by Sienna Senior Living. Management Agreement[xi] management assumed by the Scarborough Health Network.
May 31 – Camilla Care Centre Mississauga For-profit. Owned by Sienna Senior Living Management Agreement[xii] management assumed by Trillium Health Partners.
May 25 – River Glen Haven Nursing Home Sutton For-profit. Owned by Atk Care Inc. Management Order[xiii] Southlake Regional Health Centre. Extended as a Voluntary Management Agreement August 24.[xiv] |
Timing and Consistency of Management Take Over through Orders/Agreements:
The timing of management takeover through orders and agreements in Wave I was perilously late and the vast majority homes with large outbreaks were never given orders or agreements. The evidence from Wave II shows that there has not been the improvement one would expect. Despite repeated calls for the government to create capacity over the summer, including teams that are able to go into homes and take over management, provide infection control and staffing support, nothing was done. As hospitals reopened full services including surgeries, diagnostics and clinics, their capacity to continue to provide support has been greatly diminished. During its large outbreak from October – December, the Prescott and Russell residence has been unable to get a hospital team to support because there is no capacity to do so at the hospital. There is no evidence of any systematic plan to intervene in homes in crisis. In fact, it appears that the response is entirely reactive, ad hoc, and inconsistent, and mostly applied when there is enormous public pressure through media horror stories.
Tables 3 & 4 plot the timing of management orders/agreements against the tracking of the spread of COVID-19 in the homes that have been given these measures. Table 4 plots the spread of COVID-19 in the homes with large outbreaks (defined as an outbreak including more than 10 residents and staff) that did not receive management orders/agreements. Though one can readily see why the homes that have received orders were given them. It is unclear why orders are not made on more homes. It is also not clear why some of the worst performing homes have agreements rather than at minimum orders. (In our view, they should have lost their licenses to operate.) Further, though local Public Health Unit orders are publicly posted, this is not the case with the orders and agreements by the Ministry of Health and we cannot find the terms of those agreements and orders publicly available anywhere.
There remain many homes with clearly out-of-control outbreaks that do not have management orders or agreements. Among the long-term care homes currently in outbreak in Wave II with no management orders or facilitated agreements for take over:
- there is one home with more than 200 residents and staff infected;
- there are two homes with 150 – 199 residents and staff infected;
- there are five homes with 100 – 149 residents and staff infected;
- there are eight homes with 50 – 99 residents and staff infected.
There has been no clarity about how these decisions are being made:
- Why are the measures so inconsistent? Some homes have orders and some, with much worse outbreaks, have agreements. Others with terrible outbreaks have neither Management Outbreaks nor Management Agreements. See Tables 3, 4 and 5.
- Why are orders and agreements happening so late? Tyndall Nursing Home, for example, did not get a management order under 99 residents and staff were infected. Extendicare Starwood’s Management Agreement did not happen until 59 residents and staff were infected. For Extendicare West End Villa, that number was 63 when the Management Agreement occurred. At Rockcliffe Care Community, a Management Agreement was not forged until 211 residents and staff were infected and 12 had died. See Tables 3 & 4.
Table 3. Timing of Management Orders/Spread of COVID-19 in Wave II (data up to December 1): |
||
| Tyndall Nursing Home Mississauga | Millennium Trail Manor
Niagara |
Simcoe Manor Home for the Aged Beeton |
| COVID-19 Infections/Deaths:
Nov 5: 2nd outbreak started [xv] Nov 9: at least 1 resident and at least 1 staff [xvi] Nov 10: 46 residents and 9 staff [xvii] Nov 14: 53 residents and 11 staff [xviii] Nov 16: 53 residents including at least 1 death and 19 staff [xix] Nov 17: 76 residents including at least 1 death and 23 staff [xx] Nov 24: 81 residents including 7 deaths and 57 staff [xxi] Management Order – Nov 25 Nov 27: 101 residents including 23 deaths and 71 staff [xxii] Dec 1: 113 residents including 25 deaths and 74 staff [xxiii] |
COVID-19 Infections/Deaths:
Sept 29: 2nd outbreak started [xxiv] Oct 14: 9 residents including at least 1 death, and at least 1 staff member [xxv] Management Order Oct 27 Nov 4: 15 residents including 3 deaths and 14 staff [xxvi] Nov 6: 15 residents including 3 deaths and 15 staff [xxvii] Nov 15: 16 residents including 3 deaths and 15 staff [xxviii] Nov 24: 16 residents including 3 deaths and 16 staff [xxix] Nov 28: outbreak resolved [xxx]
|
COVID-19 Infections/Deaths:
Sept 29: 2nd outbreak started [xxxi] Oct 4: 4 residents including 2 deaths and 4 staff [xxxii] Oct 5: 16 residents including 2 deaths and 6 staff [xxxiii] Oct 9: 29 residents including 4 deaths and 19 staff [xxxiv] Management Order Oct 9 Oct 15: 37 residents including 5 deaths and 22 staff [xxxv] Oct 28: 40 residents including 9 deaths and 28 staff [xxxvi] Nov 8: 43 residents including 10 deaths and 31 staff [xxxvii] Nov 17: 43 residents including 10 deaths and 32 staff [xxxviii] Nov 26: outbreak resolved [xxxix] |
| Simcoe Manor Home for the Aged
Beeton |
||
| COVID-19 Infections/Deaths:
Sept 29: 2nd outbreak started [xl] Oct 4: 4 residents including 2 deaths and 4 staff [xli] Oct 5: 16 residents including 2 deaths and 6 staff [xlii] Oct 9: 29 residents including 4 deaths and 19 staff [xliii] Management Order – October 13 Oct 15: 37 residents including 5 deaths and 22 staff [xliv] Oct 28: 40 residents including 9 deaths and 28 staff [xlv] Nov 8: 43 residents including 10 deaths and 31 staff [xlvi] Nov 17: 43 residents including 10 deaths and 32 staff [xlvii] Nov 26: outbreak resolved [xlviii]
|
||
Table 4. Tracking of Large Long-Term Care Home COVID-19 Outbreaks (>10 residents and staff) with no Management Orders/Agreements facilitated by the Ministry of Long-Term Care in Wave II (data up to December 1, 2020) |
|
| Durham
Sunnycrest Nursing Home · Nov 23: outbreak started [xlix] · Dec 1: 80 residents inclu. 1 death & 5 staff [l] Eastern Ontario (excluding Ottawa) Prescott and Russell Residence LTC · Oct 7: 2nd outbreak started [li] · Oct 13: 17 residents and 8 staff members [lii] · Oct 20: 31 residents including 1 death and 17 staff members [liii] · Oct 23: The federal government had the Canadian Red Cross start supporting the Prescott and Russell Residence long-term care home [liv] · Oct 28: 72 residents including 5 deaths and 46 staff [lv] · Oct 30: 83 residents including 12 deaths and 55 staff [lvi] · Nov 6: 16 resident deaths [lvii] · Nov 12: 97 residents including 19 deaths and 62 staff [lviii] · Nov 17: 97 residents including 12 deaths and 63 staff. The number of deaths decreased as the classification of COVID-19 deaths in Ontario was changed and people who die of other conditions complicated by COVID-19 after they have recovered were no longer considered COVID-19 deaths. [lix] · Nov 18: 101 residents including 12 deaths and 64 staff [lx] · Nov 23: 104 residents including 13 deaths and 66 staff [lxi] · Nov 25: 109 residents including 14 deaths and 67 staff [lxii] Halton Allendale LTC · Nov 13: 2nd outbreak started [lxiii] · Nov 19: 1 unspecified case [lxiv] · Nov 21: 8 residents including at least 1 staff case [lxv] · Nov 26: 18 residents including 1 death, 3 staff, and 9 unspecified cases [lxvi] · Nov 30: 34 residents including 4 deaths, 4 staff, and 3 unspecified cases [lxvii]
Chartwell Waterford LTC · Oct 13: 4th outbreak started, 4 residents [lxviii] · Oct 22: 17 residents including 1 death, 1 staff and 2 unspecified cases [lxix] · Oct 28: 22 residents including 2 deaths, 3 staff and 4 unspecified cases [lxx] · Nov 3: 27 residents, 6 staff, and 11 others [lxxi] · Nov 6: 38 residents including 3 deaths, 8 staff, and 5 unspecified cases [lxxii] · Nov 9: 41 residents including 4 deaths, 9 staff, and 2 unspecified cases [lxxiii] · Nov 17: 47 residents including 7 deaths and 11 staff [lxxiv] · Nov 26: 47 residents including 8 deaths and 11 staff [lxxv] · Nov 30: 47 residents including 10 deaths and 11 staff [lxxvi] Post Inn Village LTC · Nov 13: 3rd outbreak started [lxxvii] · Nov 19: 2 residents, 2 staff, and 1 unspecified case [lxxviii] · Nov 26: 9 residents, 1 staff, and 1 other [lxxix] Wyndham Manor LTC · Oct 21: 2nd outbreak started, 1 resident [lxxx] · Nov 9: 17 residents, 5 staff, and 6 others [lxxxi] · Nov 17: 44 residents including 2 deaths, 13 staff, and 5 unspecified cases [lxxxii] · Nov 24: 49 residents (2 deaths), 15 staff [lxxxiii] · Nov 26: 53 residents including 7 deaths, 15 staff, and 8 unspecified cases [lxxxiv] · Nov 30: 56 residents including 8 deaths, 16 staff, and 5 unspecified cases [lxxxv] Hamilton Baywoods Place LTC · Nov 1: outbreak started [lxxxvi] · Nov 2: 1 staff [lxxxvii] · Nov 8: 5 residents and 2 staff [lxxxviii] · Nov 15: 17 residents including 1 death and 12 staff [lxxxix] · Nov 17: 17 residents including 1 death and 12 staff [xc] · Nov 19: 17 residents including 2 deaths and 12 staff [xci] · Nov 26: 22 residents including 2 deaths and 16 staff [xcii] · Nov 27: 23 residents including 3 deaths and 16 staff [xciii] [xciv] · Nov 30: 25 residents including 3 deaths and 17 staff [xcv] Grace Villa LTC · Nov 25: 3rd outbreak started [xcvi] · Nov 27: 5 residents [xcvii] · Nov 30: 38 residents including 1 death and 6 staff [xcviii] [xcix] Hamilton Continuing Care LTC · Oct 31: outbreak started, 1 staff [c] · Nov 5: 2 residents and 1 staff [ci] · Nov 7: 2 residents including 1 death and 1 staff [cii] · Nov 8: 10 residents including 1 death and 1 staff [ciii] · Nov 9: 10 residents including 2 deaths and 1 staff [civ] · Nov 16: 22 residents including 4 deaths and 5 staff [cv] · Nov 17: 22 residents including 4 deaths and 13 staff [cvi] · Nov 20: 22 residents including 5 deaths and 13 staff [cvii] · Nov 30: 28 residents including 7 deaths, 17 staff and 1 visitor/other case [cviii] [cix] Idlewyld Manor LTC · Nov 6: outbreak started [cx] · Nov 8: 1 staff [cxi] · Nov 18: 7 residents and 5 staff [cxii] · Nov 22: 8 residents including 1 death and 5 staff [cxiii] [cxiv] · Nov 26: 9 residents including 1 death and 5 staff [cxv] · Nov 30: 9 residents including 1 death and 8 staff [cxvi] St. Joseph’s Villa Long Term Care Home · Nov 6: 3rd outbreak started [cxvii] · Nov 8: 1 resident death [cxviii] · Nov 9: 8 residents including 1 death and 4 staff [cxix] · Nov 16: 22 residents including 1 death and 16 staff [cxx] · Nov 20: 4th outbreak started [cxxi] · Nov 26: 3rd outbreak resolved (22 residents including 1 death, 16 staff, and 1 visitor/other case) [cxxii] · Nov 26: (4th outbreak) 13 residents including 1 death and 2 staff [cxxiii] [cxxiv] · Nov 27: 13 residents including 1 death and 4 staff [cxxv] · Nov 30: 18 residents including 1 death and 9 staff [cxxvi] Willowgrove Long Term Care · Oct 22: outbreak started [cxxvii] · Oct 30: 19 residents and 15 staff [cxxviii] · Nov 2: 22 residents and 18 staff[cxxix] · Nov 5: 26 residents and 20 staff [cxxx] · Nov 6: 29 residents including 3 deaths and 20 staff [cxxxi] · Nov 8: 31 residents including 3 deaths and 20 staff [cxxxii] · Nov 11: 35 residents including 8 deaths, 20 staff and 1 essential visitor [cxxxiii] · Nov 13: 38 residents including 9 deaths, 23 staff and 1 essential visitor [cxxxiv] · Nov 17: 41 residents including 12 deaths, 26 staff and 1 essential visitor [cxxxv] · Nov 19: 43 residents including 14 deaths, 24 staff and 2 visitor/other cases [cxxxvi] · Nov 23: 48 residents including 15 deaths, 27 staff, and 2 visitor/other cases [cxxxvii] · Nov 27: 56 residents including 15 deaths, 28 staff, and 2 visitor/other cases [cxxxviii] Niagara Gilmore Lodge LTC · Oct 23: outbreak started, at least 1 staff [cxxxix] · Nov 3: 17 residents including at least 1 death and 11 staff [cxl] · Nov 6: 19 residents inclu. 6 deaths,16 staff [cxli] · Nov 14: 19 residents (7 deaths) 16 staff [cxlii] Ottawa Forest Hill LTC · Nov 12: 2nd outbreak started [cxliii] · Nov 16: 3 residents and 6 staff [cxliv] · Nov 17: 3 residents and 7 staff [cxlv] · Nov 27: 9 residents including 1 death and 15 staff [cxlvi] Longfields Manor LTC · Oct 4: outbreak started [cxlvii] · Oct 28: 15 residents and 7 staff members [cxlviii] · Nov 7: 16 residents including 2 deaths and 8 staff [cxlix] · Nov 17: 16 residents including 3 deaths and 8 staff [cl] · Nov 20: outbreak resolved, 16 residents including 4 deaths and 8 staff [cli] St. Patrick’s Home LTC · Oct 4: outbreak started [clii] · Nov 11: 2 residents and 8 staff [cliii] · Nov 16: 2 residents and 10 staff [cliv] · Nov 27: 3 residents and 10 staff [clv] The Glebe Centre Long-Term Care · Oct 25: 2nd outbreak started, 1 staff [clvi] · Oct 29: at least 19 residents including 1 death and 10 staff [clvii] · Nov 7: 23 residents including 1 death and 15 staff [clviii] · Nov 16: 23 residents including 4 deaths and 15 staff [clix] · Nov 27: 23 residents including 4 deaths and 16 staff [clx] Peel Extendicare Brampton LTC · Oct 27: 3rd outbreak started [clxi] · Nov 13: 4 staff [clxii] · Nov 24: 9 staff [clxiii] · Nov 27: 10 staff [clxiv] Hawthorn Woods Care Community LTC · Oct 31: 4th outbreak started [clxv] · Nov 24: 1 residents including 1 death and 6 staff [clxvi] · Nov 27: 7 residents including 1 death and 11 staff [clxvii] · Dec 1: 21 residents including 1 death and 14 staff [clxviii] Villa Forum LTC · Nov 2: 3rd outbreak started [clxix] · Nov 13: 1 staff [clxx] · Nov 24: 4 staff [clxxi] · Nov 27: 13 residents and 11 staff [clxxii] · Dec 1: 14 residents and 16 staff [clxxiii] Woodhall Park Care Community LTC · Oct 22: 3rd outbreak started [clxxiv] · Nov 13: 2 residents including 2 deaths and 3 staff [clxxv] · Nov 24: 2 residents including 2 deaths and 10 staff [clxxvi] · Nov 27: 4 residents including 2 deaths and 12 staff [clxxvii] · Dec 1: 6 residents including 3 deaths and 16 staff [clxxviii] Thunder Bay Southbridge Roseview Manor LTC · Nov 17: outbreak started [clxxix] · Nov 18: 1 staff [clxxx] · Nov 26: 16 residents and 4 staff [clxxxi] · Nov 30: 37 residents including 2 deaths and 15 staff [clxxxii]
|
Toronto
Craiglee Nursing Home · Oct 25: 2nd outbreak started [clxxxiii] · Oct 26: least 1 resident [clxxxiv] · Oct 31: at least 6 residents including at least 1 death and at least 1 staff [clxxxv] · Nov 1: at least 7 residents including at least 1 death and at least 1 staff [clxxxvi] · Nov 2: at least 13 residents including at least 1 death and 6 staff [clxxxvii] · Nov 8: at least 19 residents including at least 1 death and 13 staff [clxxxviii] · Nov 9: at least 34 residents including at least 1 death and 15 staff [clxxxix] · Nov 10: at least 34 residents including 5 deaths and 19 staff [cxc] · Nov 13: at least 40 residents including 6 deaths and 21 staff [cxci] · Nov 20: at least 58 residents including 10 deaths and 23 staff [cxcii] · Nov 29: at least 74 residents including 12 deaths and 32 staff [cxciii] · Dec 1: at least 86 residents including 16 deaths and 35 staff [cxciv] [cxcv] Extendicare Rouge Valley LTC · Oct 20: 2nd outbreak started [cxcvi] · Nov 4: 14 residents and 8 staff [cxcvii] · Nov 6: 29 residents and 17 staff [cxcviii] · Nov 9: at least 46 residents including at least 1 death and 18 staff [cxcix] · Nov 29: at least 63 residents including 9 deaths and 22 staff [cc] Fairview Nursing Home
Fieldstone Commons Care Community LTC
Fudger House LTC
Harmony Hills Care Community
Kennedy Lodge LTC
Lakeside LTC
Main Street Terrace LTC
North Park Nursing Home
Rockcliffe Care Community LTC
Shepherd Lodge Nursing Home · Oct 23: 2nd outbreak started [cclxxvii] · Nov 9: 9 residents including at least 1 death and 5 staff [cclxxviii] · Nov 17: 11 residents including at least 1 death and 13 staff [cclxxix] · Nov 29: 13 residents including at least 1 death and 13 staff [cclxxx] Suomi-Koti Toronto Nursing Home · Nov 9: outbreak started [cclxxxi] · Nov 20: 30 residents and 7 staff [cclxxxii] · Nov 30: 34 residents including at least 1 death and 10 staff [cclxxxiii] Vermont Square LTC
Westside Long Term Care Home · Nov 12: 4th outbreak started [ccxci] · Nov 14: 2 residents and 1 staff [ccxcii] · Nov 15: 3 residents and 3 staff [ccxciii] · Nov 20: 25 residents including at least 1 death and 8 staff [ccxciv] · Nov 26: 59 residents including 2 deaths and 23 staff [ccxcv] · Nov 30: 84 residents including 6 deaths and 42 staff [ccxcvi] Windsor Iler Lodge Long Term Care Home · Oct 30: outbreak started, 1 staff [ccxcvii] · Nov 9: 4 residents and 1 staff [ccxcviii] · Nov 12: 15 residents and 1 staff [ccxcix] · Nov 17: 17 residents and 1 staff [ccc] · Nov 27: 18 residents and 3 staff [ccci] Riverside Place LTC · Nov 20: 4th outbreak started [cccii] · Nov 21: 1 resident [ccciii] · Nov 27: 17 residents and 2 staff [ccciv] York Chartwell Pine Grove LTC
· Nov 27: 72 residents including 8 deaths and 37 staff [cccxi] King City Nursing Home · Nov 7: outbreak started [cccxii] · Nov 13: 2 staff [cccxiii] · Nov 19: 9 residents including 1 death and 6 staff [cccxiv] [cccxv] · Nov 27: 27 residents including 1 death and 18 staff [cccxvi] · Nov 30: 27 residents including 4 deaths and 20 staff [cccxvii] Langstaff Square Care Community LTC · Nov 7: 2nd outbreak started [cccxviii] · Nov 13: 2 residents and 6 staff [cccxix] · Nov 27: 8 residents and 9 staff [cccxx] Newmarket Health Centre LTC · Nov 7: outbreak started [cccxxi] · Nov 13: 1 staff [cccxxii] · Nov 27: 7 residents and 5 staff [cccxxiii] · Nov 30: 10 residents and 8 staff [cccxxiv] Villa Colombo Vaughan Di Poce Centre LTC · Nov 23: 3rd outbreak started [cccxxv] · Nov 27: 10 residents and 2 staff [cccxxvi] · Nov 30: 15 residents including 1 death and 6 staff [cccxxvii]
|
B. Improvements Followed By Lost Ground
Assessment/Testing, Laboratory Capacity
There were improvements in assessment/testing and laboratory capacity in the first wave that were lost by the failure to build enough capacity as businesses reopened and particularly once schools reopened in the fall. Severe backlogs and delays in the fall have contributed to, but we must emphasize are not the only factor in, the direct spread of COVID-19 once outbreaks were declared in long-term care homes in the fall. The failure of the provincial government to coordinate assessment/testing and laboratory capacity undoubtedly contributed to the massive community spread of the virus from September through October, which ultimately found its way into long-term care homes. Once it was in the homes, however, the available evidence shows that testing delays were one factor, but they were compounded by significant failures in infection control in the homes themselves.
In the first wave, testing capacity was ramped up and testing delays were eventually addressed. Through the summer we verified with family councils and unions that all long-term care homes about which we could find information were testing residents and staff every two weeks as per a memo from the Ministry of Long-Term Care May 31, 2020.[43] [Author’s Note: The requirement has apparently recently changed with the announcement November 20 by the Health Minister that long-term care staff in homes in the Orange, Red regions and above who provide direct care to residents will be tested weekly starting November 23.[44] ] However, we have received reports that the required bi-weekly testing did not continue in a number of homes into the fall. The failure in implementation and accountability for regular surveillance testing was compounded by the failure in provincial government planning and coordination over the summer leading to the backlogs in testing and test processing in the fall. It is not clear what the status is of testing across all homes and there is no public reporting about this. We have heard from staff working in homes and from families of residents an array of conditions. These are real-life examples from the period of September to the time of writing:
- In some homes testing of staff is voluntary and not all staff are tested. In those homes, staff told us that some staff had not been tested from the summer to late October. In other homes, staff tell us that all staff (including agency staff) are still being tested every two weeks.
- In some homes where residents have developed symptoms of COVID-19 this fall, staff and families reported to us that despite repeated requests it has taken several days to a week to get the homes to arrange testing.
- In a significant number of homes we are hearing that residents are no longer being tested until after an outbreak has been declared.
- A number of families’ and media reports reveal not only delays in getting the swabs done but then also long delays in getting test results as COVID-19 continues to spread through the homes. In just one example: in early November one family member told us that their father in a shared room with three other people, waited for days for his test results as his roommates got sick one-by-one, for example. The father has contracted COVID-19. We have heard similar accounts directly from a number of families with loved ones in homes with outbreaks. Their accounts corroborate the accounts that media have reported.
In the summer months planning should have been undertaken for the reopening of the province, capacity was not developed in the assessment centres and laboratories to deal with the influx of people requiring testing as businesses reopened, and particularly once schools reopened. This did not happen, and testing backlogs were severe through the month of September, peaking early in October, impacting the spread of COVID-19 in long-term care homes. By October 3, provincial data showed a testing backlog that numbered more than 90,000 people. Assessment centres across the province were closed for two days or more to slow the influx of new tests and enable labs to catch up. Still, testing backlogs continue at varying rates across the province and have contributed to the slowness of the response in the long-term care homes. This does not excuse home owner operators, however, who have failed to test regularly and who have failed to segregate residents who are developing symptoms from those who are not. Current numbers on testing backlogs are no longer reported.
Contact Tracing
The number of COVID-19 positive cases in Ontario’s general population escalated dramatically from September through October. The failure to create and implement a coherent plan to build capacity to handle the reopening of the economy and schools meant that Public Health Units had to abandon efforts to trace and quarantine everyone who has been exposed to the virus. On October 2, the Toronto Public Health Unit suspended contact tracing for those outside congregate care settings. The Globe and Mail obtained a copy of a Toronto Public Health e-mail, sent that day advising contact tracers to stop calling the close contacts of people who tested positive, and to pause the collection of data on where people were exposed to the virus. The email stated:
“Effective [Friday,] due to the increasing number of cases of COVID-19 in the city, Toronto Public Health is no longer able to follow up with contacts. This means that TPH will only call confirmed cases. We will not call close contacts. Confirmed cases will be asked to notify their high risk/close contacts to self-isolate”….
“Acquisition (exposure) data will also temporarily be suspended. Note TPH is also in back log of cases, of approximately 800 cases (please do not share this information with others outside this email.)”
Among the general population, positive cases increased by 24 percent in the two weeks from October 13, 2020[45], to October 28, 2020[46]. Local public health units lacked the capacity to keep up. Peel, with the highest rate of case positivity (at that point 6.5 percent of people tested were positive) did not contact trace 16.9 percent of the cases in the last week of October; Toronto did not contact trace 65 percent; for Durham the figure was 27.5 percent; and for Ottawa it was 48.8 percent.[47] There is no publicly available data on the percentage of congregate care setting (including long-term care homes) that local public health units were able to contact trace in this period. But the uncontrolled spread of the virus among the general population had a significant impact on long-term care. As seen in Graph 1, in the last two weeks of October, the number of residents and staff infected with COVID-19 in long-term care homes began to escalate more sharply and the curve steepened again through November.
Asymptomatic Staff Working
Though the rate of transmission of COVID-19 resulting from asymptomatic carriers is a matter of significant and wide-ranging debate, the fact that there is transmission is not disputed and has not been for many months. Nonetheless, provincial directives and their linked policies allow this dangerous practice, ostensibly only in rare cases and with significant controls; and these provisions have been narrowed over the months of the pandemic. According the body of directives and accompanying documents, employers are supposed to use this proviso only in rare cases and the staff are supposed to work on work isolation. This loophole is a problem, and in any case, the protections (rare use, work isolation) are not enforced. There is no public reporting or tracking of this practice, but in the first wave we believe there was improvement. This ground was lost in the second wave as the staffing emergency has intensified.
Ontario’s Directive #3, which allows employers in the homes to require COVID-positive asymptomatic staff to work, supposedly in work isolation (which is not possible for hands-on care staff in long-term care homes) was used by employers in the first wave. We heard about a number of instances both in long-term care homes and in hospitals where there were outbreaks. In these accounts from staff, work isolation was not practiced. In one case, we heard about a staff person (PSW) who was required to work despite the fact that they tested positive for COVID. The staff person posted her concerns about this on her personal social media and was fired. (Ultimately her union intervened.) As the first wave crested, we stopped hearing complaints about this practice, and, though there is no publicly-revealed data to measure it, we believed it had ceased to be used.
In the second wave, we have heard that this practice is again in use. In the month of November we have received more than five accounts that hands-on care staff are still being required to work after they have tested positive and are asymptomatic. Others report that an isolation period was required before the staff member returned to work but for some, the isolation period at their home is only 10 days, and we have one worker who reportedly was called back earlier than that.
C. Failures
Staffing
One of the most egregious failures through the COVID-19 pandemic has been the refusal by the provincial government to take action to recruit staff and improve conditions so that they can be retained to provide care. Care and infection control cannot happen without enough staff. The evidence shows that inadequate staffing has contributed to critical failures in appropriate use of PPE, cohorting and sequestering residents, horrific shortfalls in care, and gross violations of residents’ human rights and the right to consent. Despite overwhelming evidence that the staffing crisis had become an all-out emergency through the first wave of the pandemic, the provincial government refused to develop a plan to address it. In the vital summer months as there was a lull in cases, the province failed to undertake a recruitment drive and improve wages and working conditions to get more staff into the homes. When the province and public health authorities made the requirement that part-time workers with multiple jobs choose one home in which to work, they refused to make attendant requirements for homes to provide full-time work for staff and improve conditions. Instead, they deregulated the paltry existing staffing requirements, allowing homes to forgo having even one RN on site 24/7 (as is required under the Long-Term Care Homes Act) and enabling them to replace Personal Support Workers with completely untrained staff and volunteers. Agency staff were exempted from the single-site requirement and their use has grown, meaning that more staff are working in multiple sites. Home operators have not been held accountable for ensuring that even elemental care needs are met. By the end of the first wave, staffing levels in a significant number of the homes were at a critical failing point. As the second wave began, the province announced a set of piecemeal funding and training, all of which is woefully inadequate, ad hoc and/or unaccountable. As the second wave gained amplitude, staffing has collapsed in a growing number of homes. Still, no action has been taken.
The Ontario Health Coalition has measured, reported on, and advocated in every way possible to address the increasing acuity and shortfalls in care levels in long-term care for decades and we ramped up our efforts in the pandemic, conducting two staffing surveys, after Wave I and in Wave II to find and expose what is happening in the homes.
- Prior to the pandemic we released a major research report, “Situation Critical: Planning, Access, Levels of Care and Violence in Ontario’s Long-Term Care”[48] pulling together all the available data. The report found significantly increased acuity at the same time as actual hands-on care levels collected in Ministry data were declining. Access to care was worsening with increasing wait lists and disproportionate difficulties accessing long-term care for racialized and indigenous peoples. Higher levels of aggressive behaviours were not supported and more than half of the homes did not have Behavioural Supports Ontario teams. The result was increasing violence including extraordinarily high resident-on-resident homicide levels in the homes and the highest levels of staff injury of any sector in our economy.
- In 2017 we began to hear of staffing shortages that had become critical, leaving homes unable to open funded beds and unable to recruit staff even to fulfill existing shift lines (which were inadequate). Through 2018 and 2019 we held a series of round tables across the province in partnership with Unifor and we released a report on our findings in December 2019/January 2020, “Caring in Crisis: Ontario’s Long-Term Care PSW Shortage”.[49] More than 350 participants attended, including home operators and administrators, PSWs, union representatives, family councils, seniors, college staff who develop/coordinate PSW courses, local health coalitions and other long-term care advocates. What we found was disturbing: every long-term care home, in the north and in the south, rural and urban areas were reporting serious staffing shortages. Shortages meant that homes are working with one to two vacancies in every area. (That might mean that they are trying to operate 5-10 staff short, or in some larger homes, they reported that they are 20-50 PSWs short.) Work was rushed and stressful. Injuries are common. Compensation is too low for the heavy work burden. New recruits would come into homes and not last a week before leaving for other sectors. the impact of the critical staffing shortages on workload, quality of life and quality of care is profound. The report also found that as a result of these conditions there is declining enrollment in PSW courses in colleges. Most of the tools to fix this situation are in the hands of the provincial government, which, instead of acting urgently to fix the crisis, was actually cutting funding.
- After Wave I, in July, we conducted and released a survey of more than 150 long-term care staff, asking about current levels of staffing and care.[50] Conducted over the week from July 10 to July 17 in every region of Ontario, the survey found that 95 percent of the staff report that their long-term care homes are short staffed and 53% of those report that they are staff shortages every day. Sixty-three percent of the staff report that staffing levels are worse than before COVID-19 hit and 28 percent said that staffing levels are the same. (It is undisputed that there was a critical shortage already, prior to COVID-19.)
The descriptions of conditions should have resulted in immediate action by the province. Staff reported that they had worked through the first wave having been denied vacation, stat holidays and weekends under emergency orders since the beginning of the pandemic. Staff had left due to fear, injuries, lack of childcare, and the requirement to choose one home in which to work. Some homes had dozens of staff lines unfilled and many work short every day, every shift. Most described worse staffing levels on weekends and evenings and unsafe levels of staffing that are now routine. Some homes had actually cut back staff hours and were limiting overtime despite severe shortages.
When asked what care they could not provide, staff delineated a list that is deeply disturbing. More than 100 staff surveyed reported the following: baths and showers are missed regularly leaving residents without proper washing because there are too few staff to use lifts safely and because of rushing; emotional support was described as “non-existent” and most staff reported there was little to no time to do it despite residents’ loneliness and depression; there is no time to complete Activities of Daily Living (ADLs) such as brushing teeth, shaving, nail care; care was described as rushed all the time. More than 50 staff surveyed reported that there is not enough time to feed and hydrate residents properly, to reposition them so as to avoid bedsores, to toilet them when they need it. Staff reported that there are more frequent falls as a result of lack of time and supervision. A number of staff reported that there are few to no activities, no entertainment, no rehabilitation, inadequate laundry leaving shortages of linens and supplies, not enough staff to do medication carts on time, and an overall unacceptable quality of care.
- We conducted an additional survey in long-term care homes that had large outbreaks (more than 10 staff and/or residents infected) across Ontario from mid-November to December of 2020. Almost 80 percent of homes reported that they do not have enough staff to provide daily hands-on care for residents. Many staff report extraordinary workloads, many report working frequent double shifts, significant over-time requirements, staff unable to take their days off sometimes for weeks at a time, staff unable to take breaks. Vital basic care, including hygiene and feeding cannot be done. Staffing shortages mean that attempts to cohort residents to protect them from infection with COVID-19 cannot be done. Homes have resorted to measures like physical barriers, locking residents in, and taking away wheelchairs and walkers so that residents cannot get out of bed. They are being left alone in these conditions without company and care in an alarming number of homes as COVID-19 spreads through the facility.
Over almost two decades, the Ontario Health Coalition has been calling for an accountable minimum staffing standard in Ontario’s long-term care homes, based on the best evidence of the level of care needed for the acuity (that is, the complexity of the care needs) of the residents. In the years of hospital restructuring, the offload of more acute patients into long-term care settings was not matched by an increase in levels of care. Except for one brief period, the long-term care homes’ lobby, dominated by the increasingly consolidated and sophisticated for-profit chains, opposed, deflecting to “outcome-based” measures and increases in funding that were not tied to actual increases in care. (Notably the non-profit and public homes broke with this and supported the call for minimum care standards in recent years.) Governments have not only failed to implement a minimum care standard, according to the available Ministry of Health data, hands-on-care daily staffing levels actually declined even as acuity increased, leaving a widening gap between the care needs of residents and the care provided. At the same time, outcomes cannot be measured as Ontario’s long-term care life expectancy declined to approximately 18 months and as long-term care homes embraced informal policies of not transferring residents to hospitals even when they could not meet their care needs. The results of the failure can be measured in increasing violence, horror stories about bed sores and neglect, and staff injury rates. By 2017, the short falls in staffing became a crisis. Personal Support Workers, onto whom more and more complex care had been downloaded, reacted to crushing workloads and inadequate pay and working conditions by leaving the sector. Across the province, severe staffing shortages compounded already too-low staffing levels. By the time the pandemic hit, the long-term care sector was already in crisis. The evidence we have gathered through the pandemic shows that the crisis has become a full-blown emergency. On the ground it means that residents in a growing number of homes are not receiving even the elemental care that is needed to sustain life. Both their suffering and the suffering of the staff cannot be described in terms that are usually used in reports like this. Without exaggeration, the situation is nothing less than a humanitarian crisis.
While other provinces moved to address the staffing in long-term care, Ontario has done nothing substantive.
- Six months ago, at the beginning of June, Quebec’s government launched a recruitment drive backed by the full power of government and funded fully to get 10,000 PSW-equivalent workers, paid them $21 per hour for training, increased wages to $26 an hour and has deployed this small army of workers into the homes.
- British Columbia’s government took action 8 months ago to provide full time work and an increased wage of $21.75 per hour for PSWs in long-term care to stabilize the workforce.
- In contrast, Ontario’s government did nothing substantial in the summer months when there was a lull in COVID-19 cases and should have been planning for the fall. Finally in September, they announced funding and training for 2000 PSWs along with a series of piecemeal funding and training; no big recruitment drive, no full time work, no improvement in wages and working conditions that would attract people to this work. They also renewed the pandemic pay until March, but at $1 per hour less than it was in the summer. We released a brief summary of the staffing and funding announcements made in September.[51]
- In November, the provincial government announced that they had finally adopted the 4-hour minimum care standard as policy, but there were no plans to implement it. Instead, the province said that they had a goal of reaching that standard by 2024/25. There was no funding planned in the budget released this fall to move toward that standard prior to the next provincial election (nor after it). There are no targets set for any improvements in the meantime and no actual policies made to recruit, retain and increase care levels. The bottom line is that this announcement appears to be PR with no substance and a completely unaccountable timeline.
Quality & Accountability of Home Management /General Accountability, Enforcement
The pandemic has exposed a serious problem with the quality of management in a number of Ontario’s long-term care homes. Requirements that are supposed to provide protections in the case of pandemic are not followed or are meaningless. There has been a total failure of infection control leadership in a significant proportion of homes (potentially between 100 and 200 or more of the 626 homes in the province). Where the evidence is overwhelming that management is either incompetent or negligent, or both, measures have not been taken except in a very small number of homes (as per subsection A above) to intervene.
Under the Long-Term Care Homes Act (2007) and its regulation (79/10), facilities are supposed to have infection control and emergency plans (subsections 86 and 87). Staff and volunteers are to be trained in the infection control program (subsections 76 and 77). These plans are supposed to be kept up to date and tested. They include requirements for plans to prevent the transmission of infectious diseases and a plan for movement of residents out of the home in the case of an emergency. It is not clear how many homes actually have these plans at all. If they exist, they do not appear to be tested, up-to-date, include a plan for movement of residents in the case of an emergency. Clearly the plans are inadequate at best.
Also under the Long-Term Care Homes Act (2007) homes are required to have a management team including an Administrator, a Director of Nursing and Personal Care (RN), and a Medical Director (physician). They are supposed to be accountable for the operation of the home in accordance with the Act and its regulations. Throughout the pandemic, in the military reports, from family and staff accounts, the quality of the management has been extremely poor and unaccountable. There is no clear infection control team and no infection control lead in many homes. In fact, in some homes, staff have reported to us that in the pandemic, administrators are working off site. Repeated accounts tell of new staff, agency staff and volunteers deployed onto the units with little or no training. Families have seen no sign of management on the floors when the homes have fallen into chaos. Communication has been extremely poor.
Some homes have shown total incompetence or indifference to the safety of residents and staff. For most, there has been no accountability. As evidenced in detail in Subsection A above, only a handful of homes have received management orders. A small group in addition have facilitated management agreements. There has been no systematic intervention by the province and there appears to be no plan to systematically intervene to ensure that infection control teams and leadership is in place in every home. There have been no consequences for homes failing to meet even their basic requirement under the Act, “that a long-term care home is primarily the home of its residents and is to be operated so that it is a place where they may live with dignity and in security, safety and comfort and have their physical, psychological, social, spiritual and cultural needs adequately met.”
The provincial government has an array of powers under the Act to enforce these provisions. These include the inspections regime with compliance orders which have not been effectively enforced. They also include fines, management takeover, suspension of licenses, revocation of licenses, suspension of admissions. Notably, amendments that were passed by government enabling them to take a stepped approach to enforcement including serious fines up to $100,000 and license suspensions. Though these amendments were passed in 2017 under the Strengthening Quality and Accountability for Patients Act (2017) Schedule 5, the Ministry has the power to issue penalties and suspend licenses. These provisions have passed Third Reading and the bill was given Royal Assent. The specific provisions regarding fines and license suspensions are in Schedule 5 Sections 37 and 38. They have been awaiting proclamation since 2017. Throughout the entire pandemic, the Ford government has sat on these amendments and has not proclaimed them and put them into force.
In August the Quebec government addressed similar problems. They appointed a single person to be responsible and accountable for each of the 400 long-term care home’s response to COVID-19 in that province. The measures were to be put in place by the end of September and the new managers were to be paired with an infection control specialist in each home to ensure that government directives were followed.[52]
In contrast, nothing substantive has happened in Ontario. To date, no home has faced a fine, none have lost their licenses, management orders have been few, and even voluntary management agreements have been rare. There has been no accountability for even the most egregious neglect and incompetence.
Failure to Respond
During the first wave of COVID-19 we outlined what was needed to contain the spread of COVID-19 in long-term care in correspondence with Premier Doug Ford from more than 200 organizations representing more than 2 million Ontarians[53] as follows:
“We need a coherent plan from your government to stop the spread of COVID-19 in long-term care and retirement homes, including concrete measures to improve PPE supply, workplace safety and infection control, and to stabilize the workforce. We urgently need your government to take leadership and concrete coordination measures to immediately address critical staffing shortages that mean even basic daily care like feeding, bathing, hygiene, human contact are not able to be done; that palliative care needs are not being met; that care for the gravely ill is less than what is needed, as follows:
- Understaffing in long-term care is critical and must be addressed. The provincial government cannot rely on long-term care homes in crisis to get themselves out of crisis. There must be a coherent plan, led by our government, to step in with a set of coordinated, concrete measures to get staff into the homes that have lost staffing levels due to sickness, having to choose one part-time job, staff leaving etc. Leaving it to the providers to forge voluntary arrangements among themselves is not sufficient. Staff need a permanent improvement to their wages and access to full-time hours. This cannot be voluntary and there is no path to stability without the provincial government undertaking these measures. In addition to the permanent improvements to wages and access to full-time work, measures are needed while homes’ operations remain under the emergency directives. Many staff have lost significant hours of work (and thus income) as a result of the requirement to choose one work site. They are risking their health and their families to go into the homes to do care work and the loss of hours is not offset by the pandemic pay increase. Yet some homes are bringing in PSW aides, nurses and others without giving their part-time staff any increase in hours. To address this, long-term care homes must be required to increase their pay for part-timers who have been required to give up part-time work in other homes to be equivalent to full-time pay and benefits, so as not to maintain the operator’s economic incentive to limit the proportion of care delivered by full time staff. Further, the Minister of Long-Term Care must use her powers to revoke licences and appoint new management in long-term care homes that have uncontrolled outbreaks and evidence of negligence and poor practices.
- Infection control practices, workplace safety and access to PPE must be improved. Reusing surgical masks patient after patient, resident after resident, would have been totally unacceptable before COVID-19. Insufficient access to N95 masks continues to be a problem and there are shortages of other equipment. There needs to be a clear plan from the government to improve the supply of PPE or develop our own. Leaving it to industry to do voluntarily has so far been insufficient. Standards for infection control and workplace safety must be improved. Staff need the appropriate equipment, enough supply and training in order to comply with them. Staff who are infected must be supported to isolate at home. The directive allowing health care facilities to require staff to work who have tested positive for COVID-19 but are asymptomatic is dangerous and should be changed as should the loopholes that fail to stop agency staff from working at more than one location. Ongoing training and support for infection control regarding the use of PPE are needed. Testing of all residents and staff must be ongoing in long-term care homes, and completed in retirement homes and congregate care facilities (and shelters). Testing, tracking and isolating people who test positive is shown to have stopped the spread of COVID-19 in other countries. It must happen here. Access to PPE using the precautionary principle must be implemented in long-term care, hospitals, home care and across the health care system as soon as possible.
- Testing, contact tracing and isolation must be improved using our province’s full public capacity. Public hospital laboratories that are not currently doing COVID-19 testing and have unused capacity should be ramping up testing. We need a clear honest plan from the provincial government that assesses our full capacity to test (including all the public hospitals, not just those that are currently testing) and immediately ramp up to our province’s real full capacity the testing, tracking and isolating to stop the spread of COVID-19. There must be a coherent plan and immediate action to get the supply or develop it for testing kits, swabs and reagents, and transparency about what is happening with this.
- Transfers to hospitals. Where there are long-term care homes in crisis without sufficient staff to provide proper palliative and end-of-life care, as well as being unable to address the general care requirements of the residents, residents should be considered for transfer to public hospitals, which are not in crisis, for safe and proper care, subject to their right to consent.
- Bring in family caregivers and volunteer nurses as soon as possible: As soon as testing/contract tracing capacity and PPE supply are stabilized enough to do so, and as soon as training in infection control can be properly conducted, primary family caregivers need to be able to be involved as partners in their families’ care. The pool of nurses that the RNAO has recruited to help should be utilized if they have not already been.
- Institute a minimum care standard in long-term care: There has been deep consensus for decades that the rising acuity (complexity and severity of the care needs) of long-term care residents requires more care. This cannot be left to operators to do on their own, and resources — both financial and human — need to be provided to support this. There cannot be further delay in beginning to move to a 4-hour average minimum care level for residents in long-term care to protect their safety and the safety of staff.
Premier, we are also deeply concerned about our research finding that the death rates in for-profit homes are significantly higher than in non-profit homes. It is imperative that your government halt any expansion of for-profit long-term care.
The Premier referred this correspondence to the Minister of Long-Term Care who eventually sent a letter back that was, in the main, unsubstantive, referring us to the Long-Term Care Commission. Most of the measures that we called for, along with groups representing 2 million Ontarians, measures that have been called for innumerable times by experts at every level, have still not been taken.
III. Factors Contributing to the Spread of COVID-19 in the Second Wave: Case Studies
Case Study: West End Villa, Ottawa
On August 30, 2020 a second wave of COVID-19 began with the declaration of an outbreak at Extendicare’s West End Villa in Ottawa. The outbreak quickly spread through that home and across Ottawa’s long-term care homes. Though there has been no public reporting about why the spread occurred, one member of the Ontario Health Coalition Board reports that his mother’s home care PSWs in Ottawa work, at the same time, in long-term care homes in the city as agency staff. In a media report from September 29, it was revealed that among the 42 staff members who had tested positive at that point, at least one worked for an agency. It was not revealed at which other homes that agency staff person worked[54] but, notably, by mid-September eleven Ottawa long-term care homes were in outbreak[55] and Ottawa had become the epicentre of the spread of COVID-19 in Ontario’s long-term care sector.
As of November 9, eighty-seven residents and 45 staff had contracted COVID-19 in the outbreak at Extendicare’s West End Villa that started August 30. At least 20 residents had died. In total, at the time of writing, at least one hundred and thirty-two residents and staff had contracted COVID-19 in this one home.
In our tracking reports we charted the spread of the outbreak as follows:
- Aug 30: 2nd outbreak started[56]
- Sept 16: 31 residents including 5 deaths and 5 staff[57]
- Sept 18: 46 residents including 6 deaths and 17 staff[58]
- Oct 18: 84 residents including 20 deaths and 43 staff[59]
- Nov 9: 87 residents including 20 deaths and 45 staff[60]
- Nov 25: outbreak resolved, 88 residents including 20 deaths and 46 staff [61]
From the accounts of families, staff and the media, we have been able to piece together a picture of what happened as COVID-19 ripped through this home. The reports are deeply disturbing and reveal just how little had changed from the devastating failures in the first wave. The accounts of families hold that there were significant delays in getting testing done in the home itself, followed by a failure to cohort residents immediately upon development of symptoms and to isolate those who were sick from those who were not. The provincial government’s failure to build testing, lab and contact tracing capacity during the summer for the reopening of businesses and schools resulted in fatal delays in obtaining test results. Inadequate policy, poor oversight and negligible enforcement of infection control guidelines by the province and the home were apparent as staff reported inadequate access to PPE even after the home was in outbreak. Staffing levels, which were reported in on line reviews as too low prior to the pandemic,[62] crumbled during the outbreak. Care for residents, including those sick and dying with COVID-19, was horrifically inadequate. This long-term care home had been previously reported for poor or negligent care on numerous occasions. There was sufficient evidence not to take the reports of administrators about conditions in the home at face value. Yet the evidence shows that Public Health and Ministry measures to assess the home’s response were inadequate. The measures to enforce provincial guidelines, directives and policy that had by that time been created to improve infection control were inadequate. And then, finally, measures for emergency intervention were too slow and also inadequate.
Delays in testing and sequestering of residents and staff:
The provincial government’s failure to make a coherent plan to ramp up assessment/testing centre, laboratory and contact tracing capacity during the summer has had effects that can be accurately described as fatal. Inadequate capacity once businesses and schools reopened led to severe backlogs in testing and test results which were not only experienced in the general community, but also in long-term care homes. In West End Villa, according to an Ottawa Citizen report on Friday September 18, sixty tests among staff were still pending and testing was continuing among residents with 48 results pending.[63] On September 29, a memo that was given to families from the home on September 28 was reported publicly in the media. According to this report, at that point there were pending test results for 121 residents and 149 staff members.[64] Numerous public statements by Extendicare support the contention that delays in obtaining test results were hindering the home’s ability to contain the outbreak.
While inadequate laboratory capacity to process tests is undoubtedly a significant factor, accounts given by families detail a delay in conducting the testing in the home itself. Families also attest to witnessing slow and inadequate cohorting of residents even once symptoms were evident and a failure to take effective measures to stop residents from wandering into COVID “hot” zones. These are factors that had been recognized for months as significant contributors to the spread of the virus. They are the responsibility of the home operator which should have been subject to effective oversight and accountability for them.
A Postmedia report published on September 20 quotes a family member who reports lapses in testing and isolation in the home as follows:
“Lea Maurice, whose 76-year-old disabled grandmother lives in the home, says her grandmother was left in a room with a sick roommate for 24 hours after that roommate tested positive for COVID-19. The roommate had been showing signs of illness for several days before she was tested, they say. Even after the roommate tested positive, she was not immediately moved. Maurice says the home did so after family members complained.
It took another eight hours, Maurice and other family members allege, before the room was sanitized, and even then it was done with her grandmother in the room.
Maurice’s grandmother, who is not being named to protect her privacy, has now tested positive for COVID. She had to be tested twice. Officials with the home told family members that the original test was inadvertently cancelled by the lab where it was sent for processing.
Maurice said she can’t understand why it took so long to move the roommate to protect her grandmother and two other residents with whom they shared a bathroom.”[65]
Poor care, poor infection control practices, Public Health and government surveillance and interventions inadequate and too slow.
On multiple occasions, Public Health Ontario, Ottawa Public Health and the Ministry of Long-Term Care claimed that the home had sufficient PPE, sufficient staff, and was following safety protocols: contentions that are directly contradicted by accounts from families and staff with immediate knowledge of the situation. These contradictory reports raise questions about whether inspectors and officials actually went into the home and spoke with staff and residents, or whether they relied on the accounts of the home’s administration alone.
On September 11 local public health officials told the Ottawa Citizen that things had changed since the first wave and that they had ensured that West End Villa had enough PPE, and the Ministry of Long-Term Care told the same newspaper that they had ensured that the home had enough staff and proper outbreak protocols in place.[66]
Yet on Saturday, September 19 a CBC news story quoted a staff person, who spoke on the condition of anonymity for fear of losing their job, as reporting that staff working directly with residents who have COVID-19 did not have N95 masks,[67] something that had been raised repeatedly as a problem with the provincial government and public health officials. The Ottawa Citizen further reported multiple claims from staff that care levels had dropped in September to two PSWs for sixty COVID-positive residents.[68] This is a shockingly low level of staffing and means that even the most fundamental elements of care and infection control could not possibly be done.
We found a quote from Extendicare’s spokesperson on September 22 particularly disturbing. In response to the staff reports about poor access to PPE, the spokesperson is reported as saying
“N95 masks are not recommended for long-term care, but they added,
“If our staff indicate they would prefer to have an N95 mask, we make them available.””[69]
By September 22 sixty-four of the 214 residents that lived in the home at the end of August had tested positive for COVID-19 – almost one in every three – and at least 11 had died. Another 28 staff had tested positive for a total of at least 92 cases. It is hard to imagine, in this context, how the gulf between this approach and the precautionary principle recommended by the SARS Commission could be wider. This quote is revealing of both the failures of the province and the home. Even the miserly contention that staff could access N95 masks upon request, is disputed by staff. In fact, the whistleblower PSW reiterated her contention that PPE remained inadequate and expressed her fears about spread of the virus in response:
“A lot of people are getting sick really fast,” said the PSW. “Residents are getting sick. Staff are getting sick. We really think that we are not given proper personal protective equipment in order to help and to feel safe in our jobs.”[70]
On September 29 spokesperson Gloria Yip said Ottawa Public Health had been conducting daily on-site visits to West End Villa and it was also reported that the Ministry of Long-Term Care was meeting daily with the home’s licensee, the local public health unit and provincial health officials. From that surveillance, Ottawa Public Health said:
“The home has reported no critical personal protective equipment concerns or shortages at this time. The home is also addressing staffing challenges by using nurse practitioners, paramedic services and temporary staff.”
She said the provincial government has introduced “an aggressive testing, screening, and surveillance protocol, deployed specialized teams from hospitals, public health and the home care sector, recruited additional staff, and increased PPE. Long-term care homes enforce rigorous provincial standards for all public health concerns, including outbreak management systems for detecting, managing and controlling infectious disease outbreaks.”[71]
Yet, the daughter of another resident describes the conditions in which her mother Pierrette died on September 26 at West End Villa.[72]
Pierette’s room was dirty, she had excrement on her hands, there was excrement on the wall, and she had not been cleaned. Her tongue was dry, and although there were drink cartons on her table all but one had been left unopened: Pierrette, with dementia and COVID-19 was unable to open them. Despite being put into a private room for isolation as she had symptoms of COVID-19, other residents were wandering in and out, with no staff around to stop them from being exposed to the virus. There were not enough staff to provide hydration and nutrition, human company and basic care. These were the conditions in the second last week of September, three weeks after the outbreak was declared. Pierette died on Saturday September 26. Pierette’s daughter had been calling the home all morning. She finally got a call back from the nurse who apologized and said that the home was so short-staffed that she was covering two floors alone and had not been able to get into Pierette’s room until just before noon. Pierette’s family raced to the home just in time for her passing.
If, through September, Public Health officials relied on home administrators’ accounts as to what was happening in the home, which it appears they did, they should have interviewed staff and residents, and conducted on-the-ground surveillance to confirm the condition of care and infection control. There was already plenty of evidence that the home had a documented history of inadequate care, as evidenced by inspection reports and a 2018 lawsuit.
In that 2018 lawsuit, the family of a resident alleged systemic, negligent treatment, including a report that the elderly woman’s bandaged wounds were infested with maggots. In the inspection report from June 27, 2017, the most recent comprehensive annual inspection, there were problems with housekeeping, medication errors, unsafe or rough transfers of residents, call bells not being heard, residents not being assisted to eat and offensive odours so bad that one resident was unable to have visitors in their room. Between October 2018 and August 2020, there were nine critical incident reports, 10 complaints and one follow-up inspection. According to one media report:
“They detailed everything from choking incidents to residents’ blood glucose levels not being checked, to falls resulting in significant injury, more unsafe transfers to lack of infection control.” There were further reports detailing falls, injuries, drugs administered not according to instructions and failure to immediately report allegations of abuse.[73]
The order for the Ottawa Hospital to take over the home was not made until the week of September 21 at which point more than 63 residents and staff had been infected and more than 6 had died.[74] Even after the order, the infections in West End Villa more than doubled by early November. Despite the evidence of a desperate inadequacy of staffing and care, only four residents at Extendicare’s West End Villa had reportedly been hospitalized by the end of September.
On October 6 and October 9 there were two Critical Incident inspections conducted at West End Villa. The October 6 report details an incident in which a Code Blue was not called for 45 – 50 minutes after a resident had a medical emergency, during which period a staff member tried to reach the charge nurse. For this, the home received a written notification and a Compliance Order. The inspection was done September 10 – 16 and looked at that incident specifically. It was not a comprehensive inspection. The October 9 report details staff not wearing face shields/eye protection as per the IPAC program for the home. The inspection was conducted through September and into October and was Critical Incident System inspection. The home was given a written notification and a Voluntary Plan of Correction. There are no comprehensive inspections (Resident Quality Inspections RQIs) reported for this home since 2017.
Case Study: Kennedy Lodge, Toronto
As of November 16, 2020, thirty-one residents had died and 128 residents and staff were infected by COVID-19 at Kennedy Lodge long-term care home in Scarborough in a devastating outbreak that started at the beginning of October. Like at Extendicare’s West End Villa, claims from Revera Inc. which owns Kennedy Lodge and from the Minister of Long-Term Care that staffing levels were stable, even relatively high, and that PPE was not a problem, are directly contradicted by reports from the front lines. Like in West End Villa, the claims by the home administrators do not seem to be subject to rigorous independent verification and the severe staffing shortages which are described in multiple accounts, still have not been addressed.
A spokesperson for the home, owned by Revera Inc., claimed in mid-November that staffing levels were stable, staff were cohorted to specific units and there was an adequate supply of PPE.[75] His claims were echoed by the Minister of Long-Term Care Merrilee Fullerton in the Ontario Legislature on October 28. She said, “In wave 2, right now, there are no homes with critical staffing levels because we’re getting them the help that they need — including the PPE,”[76] and on Nov. 2, she said, “There are no critical situations with the homes. There are no critical staffing shortages.”[77] Regarding Kennedy Lodge in particular, the Minister told a journalist who was writing an investigative report into the conditions in the home that she had confirmed with Ministry staff that the home had sufficient PPE and they, “are in fact staffed over and above their regular staffing complement.”[78] These claims could not be more different than those of the staff working in the home.
A November 17 media report includes descriptions by a PSW who works on a COVID floor in the home:
The worker described critical staffing shortages that mean that infection control practices cannot be followed. Seven to eight staff are supposed to work on the floor, but sometimes only four show up to work and are not replaced. Staff are supposed to designated to specific floors but end up having to go between floors, including between COVID-positive and COVID-negative floors, because there are not enough of them.
The PSW went on to say that N95 masks are available but not in the specific fit-tested sizes that staff need. The staff person described shortages of PPE including gloves.
The union president described the home as short staffed prior to the pandemic, but she described the situation under outbreak in the second wave as “horribly short-staffed”.[79]
In late November we received additional accounts from staff who describe the home as short-staffed with some units hit harder than others. Multiple staff report that they have been working double-shifts and unable to get time off. Staff describe working for significant lengths of time without any days off. Agency staff are being used to fill staffing gaps, they report, sometimes without appropriate training and orientation. Further reports describe residents as sequestered so that COVID-positive residents are in specific units. However, multiple accounts hold that staff are reported to be working between both COVID-positive and COVID-negative units.
The most recent Resident Quality Inspection reported for this home is from July 2018.[80] There are no inspection reports posted at all since early February 2020 from when two Critical Incident (not comprehensive inspection) reports are posted.
The following charts the outbreak at Kennedy Lodge. There has been no Management Order for this home. Revera has put out a press release on December 10 saying it is receiving help from the Scarborough Health Network for enhanced cleaning and infection control.[81]
- Oct 2: 2nd outbreak starts [ccxxiii]
- Oct 17: 12 residents and at least 1 staff [ccxxiv]
- Oct 20: 13 residents and 8 staff [ccxxv]
- Oct 24: at least 16 residents including at least 1 death and 10 staff [ccxxvi]
- Oct 25: at least 22 residents including at least 1 death and 15 staff [ccxxvii]
- Oct 26: at least 47 residents including 4 deaths and 22 staff [ccxxviii]
- Oct 30: at least 56 residents including 6 deaths and 22 staff [ccxxix]
- Nov 3: at least 64 residents including 10 deaths and 22 staff [ccxxx]
- Nov 5: at least 76 residents including 17 deaths and 23 staff [ccxxxi]
- Nov 6: at least 83 residents including 17 deaths and 23 staff [ccxxxii]
- Nov 11: 92 residents including 29 deaths and 35 staff [ccxxxiii]
- Nov 13: 92 residents including 30 deaths and 35 staff [ccxxxiv]
Case Study: Extendicare Starwood
By mid-November, the outbreak at Extendicare’s Starwood long-term care home in Ottawa had grown to become one the province’s deadliest in the second wave. The outbreak had been simmering since September 25 and should have been stemmed quickly. Instead it took speed and has raged through the home since mid-October. A closer look at the accounts of care in the home gives some sense of what happened. Here, as in Extendicare’s West End Villa, the testing backlog played a role. Staffing shortages are described both by families and staff and have had a critical impact on the ability to sequester residents to protect them from contagion. Unlike some other homes, staff have not reported a lack of PPE, including N95 masks. Generally, it appears that families who have publicly described conditions have more favourable accounts of the home. There are mixed reviews, including a number that are positive about the home’s communications particularly in the early weeks of the outbreak. The quality of care provided by staff is described in very positive terms (in the context of describing short-staffing). The biggest issues appear to be staffing shortages, including during the period in which the Ottawa Hospital has sent in support, and a failure to quickly and effectively cohort the COVID-positive residents. In this home, as in the others, when care levels were inadequate, residents were not moved out and there were not enough staff sent in to support. (Note: The Ottawa Hospital, which has provided support is also overwhelmed, has had several COVID-19 outbreaks and has been running at more than 100 percent capacity.) The province’s failure to create a plan and build capacity during the summer for testing, contact tracing, staffing, hospital capacity, and emergency interventions is in evidence throughout this outbreak with disastrous consequences.
Like in Extendicare’s West End Villa, testing backlogs have been a significant problem. In a statement to CTV News, an Extendicare spokesperson said Starwood and some of its other long-term care homes in Ottawa have struggled with delays in getting test results.
“It has frequently taken many days to receive test results for our staff and residents. We can’t fight the virus if we don’t know where it is or who might be carrying it,” the statement says. “Delays in test results mean delays in accurate cohorting and delays in sending staff home to isolate, leaving them working in the home longer which increases the risk of spread to the residents. We had several outbreaks in our Ottawa homes that coincided with very slow lab turnaround times in September and October.”[82]
However, delays in testing and test results are not the full story about the spread of COVID-19 in this home.
Though this home appears to have had better communication with families early in the outbreak compared to other homes, corporate communications for Extendicare took over late in October and one family describes the change as follows,
“We’ve been okay with the communication but haven’t had to wait for callbacks about sick relatives as others have.🤞 We get daily emails now. Until last week the director sent them and I really appreciated all the information she provided. Last week the company’s (Extendicare) communications team took over. (I suspect the director is overwhelmed and burnt out. She works very long hours and didn’t take even 1 day off during the 1st few months of this.) The company emails are much briefer, essentially providing updated numbers and staffing info.”
Another family described the lack of communication in late October/early November as follows:
“I think a lot of families are in mental health crisis now. They just want to know what’s going on, beyond the numbers,” she said. After her sister-in-law’s son was told his mother had tested positive, there was little followup, she said.
“He got a call to say she was positive. Then he didn’t hear anything for three more days. No one would return his calls. You don’t just drop a bombshell like that without followup. It’s understandable, they are in major crisis mode there … but it’s difficult. The families are in as much distress as the people in the home.”[83]
As many accounts laud the staff as doing exceptional work, they also complain about shortages of staff and care. One family member describes the conditions of care at the end of October/early November for her grandmother who tested positive for COVID-19 and died in hospital on November 12 after the family asked the home to call an ambulance and transfer her.
“My grandmother passed away this morning. We learned she tested positive for Covid-19 on Friday evening. It wasn’t really a surprise, as the outbreak in her home (Starwood Extendicare) had spread like wildfire over the course of two short weeks.
Grandma seemed to be for the most part asymptomatic, except a low grade fever. Unfortunately, late Sunday night my aunt got a call from the ONLY NURSE ON DUTY at the home (with ~70+ active covid cases, and about 140 residents). He said he couldn’t bring her fever down, and he had had to supply oxygen, but with the best equipment they had he could only get her to 90%. He wanted to know what to do. My aunt told him to call an ambulance (a big no-no for homes – they don’t want to send their residents to hospital). This was the best decision.
At the hospital (shout out to the amazing staff at QCH!) she was put in a large negative pressure room. We were allowed to visit during end of life. Nursing staff were attentive and caring around the clock. We all agreed that although the circumstances were bad, at least she wasn’t neglected like she was at Starwood, in her final days.
I would like to be crystal clear about my feelings on this. The staff of Starwood are for the most part absolutely amazing. It is the management and executives of the company that are to blame for the woeful neglect in the homes, along with the government that has weak policies with respect to long term care, and does not adequately enforce even these weak policies that they have in place.
The ratio of PSWs to residents needs to be increased to something humane, homes need to be supplying edible and nutritious foods at every meal, homes need to ensure adequate health care, and in particular hydration! It is shameful that it even has to be said.”[84]
After her death, the family found among her possessions left at the home, the surgical masks they had bought for her protection unopened.[85]
Another family member described the situation at the beginning of November as follows:
“….As well, many residents have dementia and don’t understand the need to stay in their rooms. No home has enough staff to monitor every room to make sure no one wanders out – they simply do their best.”[86]
These reports are corroborated by staff who describe staffing shortages throughout the outbreak. Even while hospital support has been in the home, filling shifts has been difficult with staff working significant overtime to make up the shortfall. Short-staffing has resulted in inadequate infection control, particularly in cohorting or segregating COVID-positive residents to protect those who are not infected. The home did make an effort to sequester residents, moving residents to separate rooms and a COVID-wing, at least at the beginning. But staffing levels, never ideal, worsened as staff got sick or had to quarantine. As more staff and residents tested positive, staff reported to us that there were not enough staff to prevent residents from wandering. The home did, reportedly, put up yellow vinyl barriers to try to prevent wandering.
But another family report shows that the home did not only fail to prevent residents from wandering:
Rose Anne Reilly’s mother contracted COVID-19 at Extendicare Starwood in the first two weeks of November. Rose Anne describes an ongoing inadequacy of staffing, but still she was shocked and devastated by what happened to her mother, who is 104- years old. Rose Anne was informed on Friday November 13 that her mother’s roommate tested positive for COVID-19 as a result of weekly surveillance testing. Rose, who is Rose Anne’s mother, had tested negative. Despite this, the home left Rose in the same room for 48-hours (November 13- 15) with her COVID-positive roommate. Rose Anne tried to call the home but her calls went unanswered until Sunday. It was only after she says she spoke with the home’s administrator that her mother was moved later on Sunday November 15. Rose’s mother tested positive for COVID-19 the next week.
This is the spread of the virus in Extendicare Starwood which had 153 residents[87] at the beginning of the outbreak:
- Sept 25: 2nd outbreak started [cviii]
- Oct 14: 2 residents and 4 staff [cix]
- Oct 28: 50 residents including 3 deaths and 18 staff[cx]
- Nov 3: 103 residents including 8 deaths and 34 staff [cxi]
- Nov 7: 120 residents including 13 deaths and 44 staff [cxii]
- Nov 9: 129 residents including 6 deaths and 44 staff [cxiii]
- Nov 16: 134 residents including 23 deaths and 46 staff [cxiv]
It was not until the end of October when 55 residents and 20 staff members at the home had tested positive for COVID-19 and three residents had died.[88] That a “management agreement” was announced by the Ministry of Long-Term Care between the licensee and the Ottawa Hospital.[89] [90]
In late October, the Ottawa Hospital, reported that it was building a 40-bed temporary unit in the Civic Campus parking lot as hospitals across Ottawa were reporting high occupancy rates and overstretched resources at the same time [91]as the second wave was growing. This announcement followed the release of a plan in early October to open a 120-bed transitional care unit at a retirement home, to be overseen by Elisabeth Bruyere hospital, which opened in November. While Ottawa’s clinical leaders took to Twitter to warn that Ottawa was in trouble and needed more provincial support, the Ottawa Hospital was providing management and IPAC support teams to two long-term care homes, running an Assessment Centre and dealing with occupancy rates ranging from close to 100 percent to over 100 percent. Extraordinary occupancy rates in Ottawa hospitals pre-date the pandemic. It is clear that more capacity was needed to support the local health system. What is not clear is why the provincial government did not move more quickly to create capacity in the summer prior to the second wave, when options such as the model of the field hospital in Windsor and others were available and should have been deployed. Other provincial failures include, as evidenced in the other large outbreaks, the failure to build testing, lab and contact tracing capacity and the failure to recruit and train long-term care staff and improve long-term care staffing over the summer and into the fall. Finally, the failure to ensure that cohorting or sequestering of residents was done quickly and effectively, contributed to the spread of COVID-19 in Extendicare Starwood.
Case Study: Prescott and Russell Residence, Hawkesbury
The outbreak at this municipal long-term care home in Hawkesbury started October 1 and has ripped through the home for ten weeks leaving devastation in its wake. By early December, one hundred and nine of the 130 residents had contracted COVID-19 and fourteen had died. There were problems with the home’s response. But nowhere are the failures of the provincial government to build capacity to plan for the fall more in evidence. Here, as in other homes, families and residents paint a picture of agonizing staffing shortages. Unlike in other homes, the administration is much more open about the crisis and tried many options to get help. But they have been unsuccessful in getting the help needed because the hospital is overwhelmed and nothing else has been set up to provide sufficient support. In this home, the inhumanity of the decision not to allow in family caregivers and health care professionals, even as care levels collapsed, while at the same time not getting residents out to a facility where they could receive adequate care, is cast into sharp focus. At Prescott and Russell, like in so many other long-term care homes in crisis, the reluctance — even apparent refusal — of the home to send residents to hospital when they could not get adequate care in the home is in evidence.
As the outbreak progressed, Families of residents describe horrific staffing shortages as follows.
“In the early morning of Nov. 2, Alain Ménard got a call from the Prescott and Russell Residence telling him that his mom, Annette Cliff, had died. She’d only lived there for about a month, having been transferred from the nearby Hawkesbury General Hospital at the end of September into an isolated room. She was recovering from lung inflammation. While in isolation, she somehow contracted COVID-19.
“In the end, my mom was in agony,” said Ménard. “I would like that to be avoided for other residents.”
Within days of Cliff’s arrival at the home, it was in lockdown. Unable to visit, Ménard said his mom called him and reported what was happening. “She felt abandoned by the team, and she had severe bowel problems and it took a couple of hours, for instance, to clean her up, and there was some on the floor. [It] took a day for them to clean the floor,” he said.”[92]
Carlin Pethke’s account of his care in the home corroborates Alain Ménard’s report. Carlin is a 37-year old resident of the home with multiple sclerosis and in early November he and his father described his experience to the media. Carlin’s father, Rainer, reports that there were staff shortages even prior to the pandemic, but the outbreak has stretched them beyond the breaking point:
“Definitely, the staffing situation, from the point of view of the residents, is not under control,” said Rainer Pethke. “My son can’t be taken out of bed today because there’s not adequate staff.”
Both father and son say there have been many times Carlin and other residents have had to remain in bed all day and all night. He hasn’t had a real bath for about a month, and laundry and cleaning has been less frequent since the lockdown began. In some cases, residents wear hospital gowns because they have no clean clothes.
But it’s the lack of physiotherapy that’s causing the most distress for Pethke. He can’t move his legs and needs someone to bend them on a regular basis, but his physiotherapist isn’t allowed in. He said he’s asked paramedics and nurses to help him, but no one will do it. “If you didn’t move your joints for days, you would be in just excruciating pain, and that’s what’s happened to him,” Rainer Pethke said.”[93]
The home’s administrator Alexandre Gorman admitted the issues with short-staffing and insufficient care that Carlin and Rainer Pethke describe but deny that any resident has been left lying in pain, saying, “basic care” is the staff’s priority right now.” He confirmed that the physiotherapist is not allowed into the home during the outbreak. Stéphane Parisien, the chief administrative officer for the United Counties of Prescott and Russell has also openly described conditions in the home. The record of the home is not perfect by any means and the decisions of the administration are not without controversy, but unlike the spokespeople in the for-profit homes from our other case studies, he does not mince words about the staffing crisis and corroborates the accounts of families:
“With so many staff members COVID-19-positive or otherwise off sick, and others too scared to come to work, these conditions were unavoidable, according to Parisien.
“We were so short-staffed that we were having a hard time feeding everybody and changing diapers on others,” he said. “The hospital gown was the way to go to respect their dignity and not leave them friggin’ naked on the bed.”[94]
At the Prescott and Russell Residence, the county was left largely on its own grappling with the crisis. The management did ask for help but the Hawkesbury hospital was unable to provide support because it too had no staff to spare.[95] The Ministry of Long-Term Care has a complaint line and complaints are supposed to trigger inspections and follow up action. But Carlin Pethke’s father said that complaints to the Ministry have not helped.[96] The Canadian Red Cross eventually came in to help, but that help was limited and did not address the staffing shortage. In the words of Stéphane Parisien CAO of the region,
“….it wasn’t the panacea needed. “The Red Cross is not the cavalry. There are quite a number of limitations to what the Red Cross can do,” he said. “They can help us with the infectious protocols, but they don’t provide the human resources to help us feed or change residents.”
The municipality arranged for its own paramedics to come into the home to help as much as possible. As the outbreak has abated, the home has taken measures to keep rooms free for a future outbreak, and is trying to recruit and retain staff, which it says remains a struggle.
This is the trend of the virus spread at the Prescott and Russell Residence to the beginning of December:
- Oct 7: 2nd outbreak started [97]
- Oct 13: 17 residents and 8 staff members [98]
- Oct 20: 31 residents including 1 death and 17 staff members [99]
- Oct 23: The federal government had the Canadian Red Cross start supporting the Prescott and Russell Residence long-term care home [100]
- Oct 28: 72 residents including 5 deaths and 46 staff [101]
- Oct 30: 83 residents including 12 deaths and 55 staff [102]
- Nov 6: 16 resident deaths [103]
- Nov 12: 97 residents including 12 deaths and 62 staff [104]
- Nov 17: 97 residents including 12 deaths and 63 staff. The number of deaths decreased as the classification of COVID-19 deaths in Ontario was changed and people who die of other conditions complicated by COVID-19 after they have recovered were no longer considered COVID-19 deaths. [105]
- Nov 18: 101 residents including 12 deaths and 64 staff [106]
- Nov 23: 104 residents including 13 deaths and 66 staff [107]
- Nov 25: 109 residents including 14 deaths and 67 staff [108]
There are additional issues that we note in the accounts of what happened in this home. They are partly cultural and partly systemic to long-term care. First, though there was clearly inadequate care, and though capacity was not in place to bring care into the home, the home did not remove residents to hospital, even at their request. This is similar to accounts of families from other long-term care homes who have said that requests to call ambulances and remove their family member to hospital — even in the crisis with dangerous shortfalls in care — were refused or they were told that the homes were not allowed to do so. In addition, again in the context of terrible inadequacies in care, the refusal to let family caregivers into the home while volunteers from Red Cross could go in, is irrational and inhumane. It is understandable that homes are concerned about infection control, but leaving human beings without adequate food, medication, pain management, basic care and hygiene and human contact cannot be considered a viable option. Again, capacity issues are at play. The province squandered its opportunity in the summer to develop a systematic approach to building staffing capacity across the continuum from long-term care to hospitals insofar as was possible quickly, develop field hospitals or the like, build community teams to go in and help in the event of a second wave, plan emergency interventions and train family caregivers to enable them to safely resume caregiving and help.
Here is a final summary from the accounts of the families:
Despite the changes to the provincial directive and policies allowing essential caregivers into Ontario’s long-term care homes, no family members were allowed into the Prescott Russell Residence.
“Essential caregivers will require specialized classes before they’re allowed inside. But due to the outbreak, those classes have yet to start, and [home administrator Alexendre] Gorman said there are also concerns about liability. The Pethke family agreed to sign liability waivers, but they haven’t been allowed in to help Carlin, and are only able to stay in touch by phone.”To see them in person would just perk me up, and them too … plus they’re going to help a little bit to make me better and ease off on the workload of the nurses and PSWs,” Carlin Pethke said.”[109]
Alain Ménard’s mother, Annette Cliff, desperate for help, took matters into her own hands:
“Ménard said the lack of communication left the families in the dark. “Calls were never returned. The few times that we did talk with them, they didn’t have much information for us. It was very frustrating,” he said.
Toward the end of her life, [Annette] called 911 to get an ambulance to bring her to the Hawkesbury General because she felt she wasn’t treated properly, and [the home] refused access to the ambulance,” he said. Administrators said they were unable to comment on that 911 call. Ménard’s family wants answers as to why things happened the way they did.
County CAO Parisien said, “Are there things we should have done better? Yes, in terms of communications, we should have communicated to the families in a faster, more efficient way. But it was overwhelming.”[110]
—————-
Endnotes
[1] https://ottawacitizen.com/news/forty-seven-new-covid-19-cases-in-ottawa
[2]https://www.google.com/search?q=extendicare+west+end+villa&rlz=1C1CHBD_enCA886CA886&oq=Extendicare+West+End+Villa&aqs=chrome.0.0i355i457j46i175i199j0l4j69i60.4696j0j15&sourceid=chrome&ie=UTF-8#lrd=0x4cce072a23be0333:0x80e10819c3277b2f,1,,,
[3] Public Health Ontario data as at December 1.
[4] These two are Garden City Manor, Niagara, June 5 – August 4, 11 residents (including 3 deaths) and 10 staff; Nisbet Lodge, Toronto, June 10 – August 7, 28 residents (including 8 deaths) and 25 staff. We have tracked data from Public Health Ontario, the Ministry of Long-Term Care database, and local Public Health Units throughout the pandemic, including the summer months and the size of outbreaks in the summer is included in our regular tracking reports here: https://www.ontariohealthcoalition.ca/index.php/resources-analysiscovid-19-resources-analysis-of-the-ford-governments-response/
[5] https://files.ontario.ca/moh-covid-19-report-en-2020-09-02.pdf
[6] https://files.ontario.ca/moh-covid-19-report-en-2020-12-02.pdf
[7] https://files.ontario.ca/moh-covid-19-report-en-2020-11-01.pdf
[8] https://www.ontariohealthcoalition.ca/index.php/report-tracking-the-spread-of-covid-19-sharp-escalation-in-large-covid-19-outbreaks-in-health-care-settings-data-updated-to-december-1/
[9] https://www.ontario.ca/page/how-ontario-is-responding-covid-19#section-0 accessed December 3, 2020.
[10] Ibid accessed August 24, 2020.
[11] https://files.ontario.ca/moh-covid-19-report-en-2020-11-25.pdf
[12] https://files.ontario.ca/moh-covid-19-report-en-2020-12-02.pdf
[13] https://www.cdc.gov/mmwr/volumes/69/wr/mm6939e1.htm
[14] https://www.cbc.ca/news/canada/toronto/covid-19-ontario-cases-data-1.5726687 and https://twitter.com/DFisman/status/1305834334671302656
[15] This is visibly depicted in the graphs labelled “Figure 4a. Rate of confirmed cases of COVID-19 per 100,000 population by age group and public health unit reported week: Ontario” in the Ontario weekly epidemiologic summaries here: https://covid-19.ontario.ca/covid-19-epidemiologic-summaries-public-health-ontario#weekly
[16] https://www.ontario.ca/page/how-ontario-is-responding-covid-19#section-1
[17] https://files.ontario.ca/moh-covid-19-report-en-2020-11-18.pdf
[18] The Public Health Ontario database had both a significant time lag and the numbers of cases were very different than our calculations which totalled up the number of cases in each outbreak report and tracked them week by week from the local Public Health Units. By June, the Ministry of Long-Term Care data set was added to the public reporting by Public Health Ontario and the Ontario Ministry of Health, and the two sets of data had significantly different numbers throughout the period in which the information was reported. We tracked the numbers for the three data sets: ours, Public Health Ontario’s and the Ministry of Long-Term Care’s. In late August – early September, Public Health Ontario changed its database. Since then we have been using Public Health Ontario data.
[19] http://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/directives/LTCH_HPPA.pdf
In the earlier versions of Directive #3 at the end of May (updates were issued May 21 and again May 23) that had different language in this section than the June 10 version. Those were updates that changed the initial version of Directive 3 issued in March. Please refer to the various versions of the Directive to see the language changes.
[20] Under Directive #3 (1) Admissions may take place during an outbreak only if it is approved by the local public health unit, and there is concurrence between the home, public health and hospital.
[21] http://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/directives/LTCH_HPPA.pdf
[22] This measure was originally made under the emergency act then continued under the Reopening Ontario O. Reg. 146/20: Limiting Work to a Single Long-Term Care Home https://www.ontario.ca/laws/regulation/200146
[23] O. Reg. 95/20: Streamlining Requirements for Long-Term Care Homes
https://www.ontario.ca/laws/regulation/200095
[24] https://news.ontario.ca/en/release/59466/ontario-supports-management-agreement-between-lakeridge-health-and-sunnycrest-nursing-home
[25] Ibid.
[26] This regulation can be found under the Reopening Ontario (A Flexible Response to COVID-19) Act (2020) here: https://www.ontario.ca/laws/regulation/200210
[27] Ontario Long-Term Care Homes Act (2007) Section 5. https://www.ontario.ca/laws/statute/07l08
[28] In addition, under the Strengthening Quality and Accountability for Patients Act (2017) Schedule 5, the Ministry has the power to issue penalties and suspend licenses. These provisions have passed Third Reading and the bill was given Royal Assent. The specific provisions regarding fines and license suspensions are in Schedule 5 Sections 37 and 38. They have been awaiting proclamation since 2017.
[29] https://www.ontario.ca/laws/statute/07l08
[30] https://www.ontario.ca/laws/statute/07l08
[31] Ontario Reg. 210/20 under the Emergency Management and Civil Protection Act. Continued under the Reopening Ontario (A Flexible Response to COVID-19) Act (2020) Reg. 210/20 https://www.ontario.ca/laws/regulation/200210
[32] https://news.ontario.ca/en/release/59340/ontario-orders-new-management-at-mississauga-long-term-care-home
[33] https://news.ontario.ca/en/release/58963/new-management-ordered-at-niagara-falls-ontario-long-term-care-home
[34] https://news.ontario.ca/en/release/58783/new-management-ordered-at-beeton-ontario-long-term-care-home
[35] https://www.villacharities.com/long-term-care/villa-colombo/management/
[36] https://news.ontario.ca/en/release/57645/hospital-assumes-management-of-villa-colombo-in-north-york
[37] https://news.ontario.ca/en/release/57115/hospital-assumes-management-of-woodbridge-vista-care-community-in-vaughan
[38] https://news.ontario.ca/en/release/57087/new-management-appointed-at-kitchener-long-term-care-home
[39] https://news.ontario.ca/en/release/57011/hospitals-assume-management-of-two-long-term-care-homes
[40] https://southlake.ca/wp-content/uploads/2020/06/MMO-under-EO_River-Glen_FINAL-May-25-2020.pdf
[41] https://georginapost.com/2020/08/24/province-extends-southlakes-takeover-of-river-glen-haven-by-30-days/
[42] https://news.ontario.ca/en/release/59466/ontario-supports-management-agreement-between-lakeridge-health-and-sunnycrest-nursing-home
[43] http://health.gov.on.ca/en/pro/programs/ltc/memo_20200716.aspx
[44] https://news.ontario.ca/en/release/59305/ontario-taking-further-action-to-stop-the-spread-of-covid-19
[45] Weekly Epidemiologic Summary. Public Health Ontario. October 13 2020. https://www.publichealthontario.ca/-/media/documents/ncov/epi/2020/10/covid-19-weekly-epi-summary-report-oct-10.pdf?la=en
[46] Weekly Epidemiologic Summary. Public Health Ontario. October 28 2020. https://www.publichealthontario.ca/-/media/documents/ncov/epi/covid-19-weekly-epi-summary-report.pdf?la=en
[47] Declerq, Katherine. New modelling shows where COVID-19 outbreaks are happening in hot spots CTV Toronto October 29 2020 https://toronto.ctvnews.ca/new-modelling-shows-where-covid-19-outbreaks-are-happening-in-hot-spots-1.5165764
[48] The report was released in January 2019 and is here: https://www.ontariohealthcoalition.ca/index.php/situation-critical-planning-access-levels-of-care-and-violence-in-ontarios-long-term-care/
[49] https://www.ontariohealthcoalition.ca/index.php/report-caring-in-crisis-ontarios-long-term-care-psw-shortage/
[50] https://www.ontariohealthcoalition.ca/index.php/release-report-95-of-ontario-long-term-care-staff-report-staffing-shortages-leaving-basic-care-needs-unmet-health-coalition-releases-staffing-survey-calling-for-ford-government-to-take-action/
[51] https://www.ontariohealthcoalition.ca/index.php/health-coalition-calls-for-government-to-flow-urgently-needed-money-to-hospitals-and-long-term-care-staffing-announcements-far-less-than-other-provinces/
[52] https://nationalpost.com/pmn/news-pmn/canada-news-pmn/quebec-reports-46-new-covid-19-cases-six-additional-deaths-linked-to-virus
[53] The complete Open Letter is here: https://www.ontariohealthcoalition.ca/index.php/open-letter-open-letter-to-doug-ford-signed-by-100-orgs-1-5-million-ontarians-ltc-commission-immediate-measures/
[54] https://www.msn.com/en-ca/news/canada/west-end-villa-reports-two-more-covid-related-deaths/ar-BB19vQsg
[55] https://ottawacitizen.com/news/forty-seven-new-covid-19-cases-in-ottawa
[56] Daily COVID-19 Dashboard. Ottawa Public Health. September 14 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[57] Daily COVID-19 Dashboard. Ottawa Public Health. September 16 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[58] Daily COVID-19 Dashboard. Ottawa Public Health. September 18 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[59] Daily COVID-19 Dashboard. Ottawa Public Health. October 19 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[60] Daily COVID-19 Dashboard. Ottawa Public Health. November 9 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[61] COVID-19 Update. Ottawa Health Unit November 27 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[62] https://www.google.com/search?q=extendicare+west+end+villa+tests+pending&rlz=1C1CHBD_enCA886CA886&oq=Extendicare+west+end+villa&aqs=chrome.0.69i59j69i57j46i175i199i457j0l2j69i60l3.5665j1j7&sourceid=chrome&ie=UTF-8#lrd=0x4cce072a23be0333:0x80e10819c3277b2f,1,,,
[63] https://ottawacitizen.com/news/local-news/two-more-residents-die-in-covid-19-outbreak-at-extendicare-west-end-villa
[64] https://www.msn.com/en-ca/news/canada/west-end-villa-reports-two-more-covid-related-deaths/ar-BB19vQsg
[65] https://www.sprucegroveexaminer.com/news/provincial/long-term-care-we-said-we-would-never-let-this-happen-again/wcm/4251ce72-b85c-4fe5-860e-0f821f49a8b3
[66] https://ottawacitizen.com/news/local-news/what-is-the-plan-ottawa-long-term-care-outbreak-raises-fears-about-readiness-for-next-wave-of-covid-19
[67] https://www.cbc.ca/news/canada/ottawa/ontario-premier-west-end-villa-outbreak-covid-19-1.5730766
[68] https://ottawacitizen.com/news/local-news/public-health-orders-hospital-to-take-over-management-of-long-term-care-homes and https://ottawacitizen.com/news/local-news/they-are-afraid-worker-says-staff-fear-showing-up-at-west-end-villa-long-term-care-home
[69] https://ottawacitizen.com/news/local-news/public-health-orders-hospital-to-take-over-management-of-long-term-care-homes
[70] Ibid.
[71] https://ottawacitizen.com/news/local-news/seniors-group-files-lawsuit-calls-on-province-to-stop-admissions-at-west-end-villa
[72] https://podcasts.apple.com/ca/podcast/her-mother-survived-first-wave-in-long-term-care-then/id1439621628?i=1000493751849
[73] https://ottawacitizen.com/news/local-news/seniors-group-files-lawsuit-calls-on-province-to-stop-admissions-at-west-end-villa
[74] https://www.msn.com/en-ca/news/canada/west-end-villa-reports-two-more-covid-related-deaths/ar-BB19vQsg
[75] https://www.huffingtonpost.ca/entry/covid-care-home-deaths-kennedy-lodge-scarborough_ca_5fb43bd2c5b66cd4ad3faeb8
[76] http://hansardindex.ontla.on.ca/hansardespeaker/42-1/l201-3_84.html
[77] http://hansardindex.ontla.on.ca/hansardespeaker/42-1/l203-4_39.html
[78] https://www.huffingtonpost.ca/entry/covid-care-home-deaths-kennedy-lodge-scarborough_ca_5fb43bd2c5b66cd4ad3faeb8
[79] https://www.huffingtonpost.ca/entry/covid-care-home-deaths-kennedy-lodge-scarborough_ca_5fb43bd2c5b66cd4ad3faeb8
[80] http://publicreporting.ltchomes.net/en-ca/homeprofile.aspx?Home=2654&tab=1
[81] https://cdn.reveraliving.com/-/media/files/covid-19/dec-2020/media-statement-kennedy-lodge-scarborough-ltc-dec10-2020.pdf?rev=ed2c9a1a57434d89a95e3b6b82173a9b&hash=D6E654D8AB6E366B28E5D7B6B220C58C&_ga=2.239363075.1484232072.1607960605-2022651287.1604323814
[82] https://ottawa.ctvnews.ca/extendicare-says-delays-in-getting-test-results-contributed-to-covid-19-outbreak-at-starwood-1.5189029
[83] https://ottawacitizen.com/news/local-news/ottawas-extendicare-starwood-covid-19-outbreak-the-worst-in-the-province
[84] https://www.facebook.com/groups/322186134878345/permalink/1089111918185759 Facebook post from Sara Rodney November 12, 2020.
[85] Facebook post from Sara Rodney, November 28, 2020.
[86] Facebook post from Susan Coles November 3, 2020.
[87] https://ottawacitizen.com/news/local-news/ottawas-extendicare-starwood-covid-19-outbreak-the-worst-in-the-province
[88] https://ottawa.ctvnews.ca/extendicare-says-delays-in-getting-test-results-contributed-to-covid-19-outbreak-at-starwood-1.5189029
[89] https://ottawa.ctvnews.ca/ottawa-hospital-providing-management-support-to-ottawa-long-term-care-home-1.5169423
[90] https://news.ontario.ca/en/release/58989/the-ottawa-hospital-and-extendicare-starwood-enter-into-management-agreement
[91] https://ottawacitizen.com/news/local-news/hospitals-facing-enormous-pressure-as-crowding-leads-to-calls-for-stricter-lockdown
[92] https://www.cbc.ca/news/canada/ottawa/prescott-russell-residence-continuing-outbreak-administration-overwhelmed-1.5828299
[93] https://www.cbc.ca/news/canada/ottawa/young-long-term-care-resident-hawkesbury-reveals-issues-during-outbreak-1.5787056
[94] https://www.cbc.ca/news/canada/ottawa/prescott-russell-residence-continuing-outbreak-administration-overwhelmed-1.5828299
[95] https://www.cbc.ca/news/canada/ottawa/prescott-russell-residence-continuing-outbreak-administration-overwhelmed-1.5828299 https://www.cbc.ca/news/canada/ottawa/young-long-term-care-resident-hawkesbury-reveals-issues-during-outbreak-1.5787056
[96] https://www.cbc.ca/news/canada/ottawa/young-long-term-care-resident-hawkesbury-reveals-issues-during-outbreak-1.5787056
[97] Racine, Francis. Hawkesbury LTC outbreak fuels increase in EOHU COVID-19 cases. The Cornwall Standard Freeholder. October 13 2020. https://www.standard-freeholder.com/news/local-news/hawkesbury-ltc-outbreak-fuels-increase-in-eohu-covid-19-cases
[98] Racine, Francis. Hawkesbury LTC outbreak fuels increase in EOHU COVID-19 cases. The Cornwall Standard Freeholder. October 13 2020. https://www.standard-freeholder.com/news/local-news/hawkesbury-ltc-outbreak-fuels-increase-in-eohu-covid-19-cases
[99] Morgan, James. Prescott-Russell Residence COVID-19 case count remains at 48, four other outbreaks in effect across EOHU territory. The Review. October 20 2020. https://thereview.ca/2020/10/20/prescott-russell-residence-covid-19-case-count-remains-at-48-four-other-outbreaks-in-effect-across-eohu-territory/
[100] Canadian Red Cross Supporting Long-Term Care Home in Hawkesbury. Ontario Newsroom. October 23 2020. https://news.ontario.ca/en/release/58920/canadian-red-cross-supporting-long-term-care-home-in-hawkesbury
[101] Morgan, James. 38 residents remain positive for COVID-19 at Prescott and Russell Residence. The Review. October 28 2020. https://thereview.ca/2020/10/28/38-residents-remain-positive-for-covid-19-at-prescott-and-russell-residence/
[102] Morgan, James. Deaths due to COVID-19 at Prescott and Russell Residence reach 12, Hawkesbury business cases confirmed, town leads EOHU in active cases. The Review. November 2 2020. https://thereview.ca/2020/11/02/deaths-due-to-covid-19-at-prescott-and-russell-residence-reach-12-hawkesbury-business-cases-confirmed-town-leads-eohu-in-active-cases/
[103] Morgan, James. Prescott and Russell Residence COVID-19 outbreak results in 16 deaths, EOHU a yellow zone as of Saturday. The Review. November 6 2020. https://thereview.ca/2020/11/06/prescott-and-russell-residence-covid-19-outbreak-results-in-16-deaths-eohu-a-yellow-zone-as-of-saturday/
[104] Morgan, James. Eight new cases of COVID-19 at Prescott and Russell Residence. The Review. November 12 2020. https://thereview.ca/2020/11/12/eight-new-cases-of-covid-19-at-prescott-and-russell-residence/
[105] Morgan, James. 29 cases of COVID-19 remain active at Prescott and Russell Residence, 141 active cases across EOHU territory. The Review. November 17 2020. https://thereview.ca/2020/11/17/29-cases-of-covid-19-remain-active-at-prescott-and-russell-residence-141-active-cases-across-eohu-territory/
[106] Morgan, James. New COVID-19 cases at Prescott and Russell Residence, and an explanation of confusing case numbers. The Review. November 18 2020. https://thereview.ca/2020/11/18/new-covid-19-cases-at-prescott-and-russell-residence-and-an-explanation-of-confusing-case-numbers/
[107] Morgan, James. 106 active cases of COVID-19 across EOHU territory while Residence outbreak continues. The Review. November 24 2020. https://thereview.ca/2020/11/24/106-active-cases-of-covid-19-across-eohu-territory-while-residence-outbreak-continues/
[108] Morgan, James. One death, new cases of COVID-19 at Prescott and Russell Residence. The Review. November 25 2020. https://thereview.ca/2020/11/25/one-death-new-cases-of-covid-19-at-prescott-and-russell-residence/
[109] https://www.cbc.ca/news/canada/ottawa/young-long-term-care-resident-hawkesbury-reveals-issues-during-outbreak-1.5787056
[110] https://www.cbc.ca/news/canada/ottawa/prescott-russell-residence-continuing-outbreak-administration-overwhelmed-1.5828299
[i] https://news.ontario.ca/en/release/59459/ontario-supports-management-agreement-between-southlake-regional-health-centre-and-king-city-lodge-n
[ii] https://news.ontario.ca/en/release/59409/ontario-supports-management-agreements-at-two-long-term-care-homes
[iii] Ibid.
[iv] https://news.ontario.ca/en/release/58989/the-ottawa-hospital-and-extendicare-starwood-enter-into-management-agreement
[v] https://news.ontario.ca/en/release/58724/unity-health-toronto-hospital-and-norwood-nursing-home-enter-into-management-agreement
[vi] https://news.ontario.ca/en/release/58521/the-ottawa-hospital-enters-into-management-agreements-with-extendicare-west-end-villa-and-extendicar
[vii] https://news.ontario.ca/en/release/58521/the-ottawa-hospital-enters-into-management-agreements-with-extendicare-west-end-villa-and-extendicar
[viii] https://www.shn.ca/news/scarborough-health-network-enters-management-agreement-with-extendicare-guildwood/
[ix] https://hawthorneplacecarecentre.ca/wp-content/uploads/sites/10/2020/06/NYGH_Hawthorne-Letter-to-families_June-17-2020.pdf
[x] https://www.lakeridgehealth.on.ca/en/news/index.aspx?_mid_=2095&newsId=845ed91c-09c2-4353-a550-5376568982ad
[xi] https://www.shn.ca/news/shn-assumes-temporary-management-of-altamont-care-community/
[xii] https://trilliumhealthpartners.ca/camilla/Documents/June-15-Initial-Report-of-the-Temporary-Manager.pdf
[xiii] https://southlake.ca/wp-content/uploads/2020/06/MMO-under-EO_River-Glen_FINAL-May-25-2020.pdf
[xiv] https://georginapost.com/2020/08/24/province-extends-southlakes-takeover-of-river-glen-haven-by-30-days/
[xv] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 17 2020. https://peelregion.ca/coronavirus/case-status/
[xvi] Active COVID-19 Outbreaks in Toronto Retirement Homes and Hospitals, November 16 2020. City of Toronto. November 16 2020. https://www.toronto.ca/home/covid-19/covid-19-latest-city-of-toronto-news/covid-19-status-of-cases-in-toronto/
[xvii] Active COVID-19 Outbreaks in Toronto Retirement Homes and Hospitals, November 16 2020. City of Toronto. November 16 2020. https://www.toronto.ca/home/covid-19/covid-19-latest-city-of-toronto-news/covid-19-status-of-cases-in-toronto/
[xviii] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 14 2020. https://peelregion.ca/coronavirus/case-status/
[xix] Long-Term Care Home COVID-19 Data. Government of Ontario. November 16 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[xx] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 17 2020. https://peelregion.ca/coronavirus/case-status/
[xxi] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 24 2020. https://peelregion.ca/coronavirus/case-status/
[xxii] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 27 2020. https://peelregion.ca/coronavirus/case-status/
[xxiii]Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. December 1 2020. https://peelregion.ca/coronavirus/case-status/
[xxiv] Health Care Facility Outbreaks. Niagara Region Health. October 14 2020. https://www.niagararegion.ca/health/inspect/outbreaks.aspx
[xxv] Long-Term Care Home COVID-19 Data. Government of Ontario. October 15 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[xxvi] Mitchell, Don. Niagara EMS reports multiple coronavirus cases among workers. Global News. November 4 2020. https://globalnews.ca/news/7441920/niagara-ems-coronavirus-cases-workers-covid-19/?fbclid=IwAR2wXUx94DptZ9qoOwQI2JVb_uYdWzRTft0EPAWE0s8jC1oIk13IHggFSXg
[xxvii] LaFleche, Grant. Six Gilmore Lodge residents with COVID-19 have died. St. Catharines Standard. November 6 2020. https://www.orangeville.com/news-story/10241248-six-gilmore-lodge-residents-with-covid-19-have-died/
[xxviii] Mitchell, Don. Coronavirus: Hamilton reported 74 new COVID-19 cases on the weekend, 5 deaths. Global News. November 15 2020. https://globalnews.ca/news/7463827/coronavirus-cases-hamilton-weekend-nov-15/
[xxix] Mitchell, Don. Coronavirus: Hamilton reports 26 new COVID-19 cases, 3 deaths. Global News. November 24 2020. https://globalnews.ca/news/7481172/coronavirus-hamilton-cases-nov-24/
[xxx] Walter, Karena. Outbreak lasting two months at Millennium Trail Manor declared over. Welland Tribune. November 28 2020. https://www.wellandtribune.ca/news/niagara-region/2020/11/28/outbreak-lasting-two-months-at-millennium-trail-manor-declared-over.html
[xxxi] Current Outbreaks. Simcoe Muskoka District Health Unit. October 14 2020. http://www.simcoemuskokahealth.org/JFY/HPPortal/ResourcesTools/OutbreakResources/CurrentOutbreaks
[xxxii] Morris, Siobhan. Two residents of Simcoe Manor die in the midst of COVID-19 outbreak. Barrie CTV News. October 4 2020. https://barrie.ctvnews.ca/two-residents-of-simcoe-manor-die-in-the-midst-of-covid-19-outbreak-1.5132730
[xxxiii] Prichard, Brad. COVID-19 outbreak at Simcoe Manor in Beeton grows to 16 residents, six staff members. Alliston Herald. October 5 2020. https://www.simcoe.com/news-story/10216807-covid-19-outbreak-at-simcoe-manor-in-beeton-grows-to-16-residents-six-staff-members/
[xxxiv] Phillips, Kim. Nearly 50 people at Simcoe Manor test positive, four have died. Barrie CTV News. https://barrie.ctvnews.ca/nearly-50-people-at-simcoe-manor-test-positive-four-have-died-1.5140180
[xxxv] Goldfinger, Daina. Almost 60 COVID-19 cases, five deaths now reported at Simcoe Manor long-term care home. October 15 2020. https://globalnews.ca/news/7398844/simcoe-manor-long-term-care-covid-19/
[xxxvi] Engel, Erika. Five Barrie residents among 21 COVID cases reported in Simcoe County today. BarrieToday.com. October 28 2020. https://www.barrietoday.com/coronavirus-covid-19-local-news/five-barrie-residents-among-21-covid-cases-reported-in-simcoe-county-today-2830681
[xxxvii] Morris, Siobhan. More Simcoe Manor staffers test positive for COVID-19. CTV News. November 8 2020. https://barrie.ctvnews.ca/more-simcoe-manor-staffers-test-positive-for-covid-19-1.5180234
[xxxviii] Engel, Erika. There are six active COVID outbreaks at long-term care/retirement homes in Simcoe County. Collingwoodtoday.ca. November 17 2020. https://www.collingwoodtoday.ca/coronavirus-covid-19-local-news/there-are-six-active-covid-outbreaks-at-long-term-care-facilities-in-simcoe-county-2886872
[xxxix] Goldfinger, Daina. Coronavirus: Simcoe Manor nursing home outbreak declared over. Global News. November 27 2020. https://globalnews.ca/news/7488081/simcoe-manor-coronavirus-outbreak-over/
[xl] Current Outbreaks. Simcoe Muskoka District Health Unit. October 14 2020. http://www.simcoemuskokahealth.org/JFY/HPPortal/ResourcesTools/OutbreakResources/CurrentOutbreaks
[xli] Morris, Siobhan. Two residents of Simcoe Manor die in the midst of COVID-19 outbreak. Barrie CTV News. October 4 2020. https://barrie.ctvnews.ca/two-residents-of-simcoe-manor-die-in-the-midst-of-covid-19-outbreak-1.5132730
[xlii] Prichard, Brad. COVID-19 outbreak at Simcoe Manor in Beeton grows to 16 residents, six staff members. Alliston Herald. October 5 2020. https://www.simcoe.com/news-story/10216807-covid-19-outbreak-at-simcoe-manor-in-beeton-grows-to-16-residents-six-staff-members/
[xliii] Phillips, Kim. Nearly 50 people at Simcoe Manor test positive, four have died. Barrie CTV News. https://barrie.ctvnews.ca/nearly-50-people-at-simcoe-manor-test-positive-four-have-died-1.5140180
[xliv] Goldfinger, Daina. Almost 60 COVID-19 cases, five deaths now reported at Simcoe Manor long-term care home. October 15 2020. https://globalnews.ca/news/7398844/simcoe-manor-long-term-care-covid-19/
[xlv] Engel, Erika. Five Barrie residents among 21 COVID cases reported in Simcoe County today. BarrieToday.com. October 28 2020. https://www.barrietoday.com/coronavirus-covid-19-local-news/five-barrie-residents-among-21-covid-cases-reported-in-simcoe-county-today-2830681
[xlvi] Morris, Siobhan. More Simcoe Manor staffers test positive for COVID-19. CTV News. November 8 2020. https://barrie.ctvnews.ca/more-simcoe-manor-staffers-test-positive-for-covid-19-1.5180234
[xlvii] Engel, Erika. There are six active COVID outbreaks at long-term care/retirement homes in Simcoe County. Collingwoodtoday.ca. November 17 2020. https://www.collingwoodtoday.ca/coronavirus-covid-19-local-news/there-are-six-active-covid-outbreaks-at-long-term-care-facilities-in-simcoe-county-2886872
[xlviii] Goldfinger, Daina. Coronavirus: Simcoe Manor nursing home outbreak declared over. Global News. November 27 2020. https://globalnews.ca/news/7488081/simcoe-manor-coronavirus-outbreak-over/
[xlix] Health Department’s COVID-19 Tracker. Durham Region. December 1 2020. https://app.powerbi.com/view?r=eyJrIjoiNDZkYzgzN2YtNGM2Yi00ZTQ0LTkzOTUtY2IwOTlhNzlmMWE2IiwidCI6IjUyZDdjOWMyLWQ1NDktNDFiNi05YjFmLTlkYTE5OGRjM2YxNiJ9
[l] Health Department’s COVID-19 Tracker. Durham Region. December 1 2020. https://app.powerbi.com/view?r=eyJrIjoiNDZkYzgzN2YtNGM2Yi00ZTQ0LTkzOTUtY2IwOTlhNzlmMWE2IiwidCI6IjUyZDdjOWMyLWQ1NDktNDFiNi05YjFmLTlkYTE5OGRjM2YxNiJ9
[li] Racine, Francis. Hawkesbury LTC outbreak fuels increase in EOHU COVID-19 cases. The Cornwall Standard Freeholder. October 13 2020. https://www.standard-freeholder.com/news/local-news/hawkesbury-ltc-outbreak-fuels-increase-in-eohu-covid-19-cases
[lii] Racine, Francis. Hawkesbury LTC outbreak fuels increase in EOHU COVID-19 cases. The Cornwall Standard Freeholder. October 13 2020. https://www.standard-freeholder.com/news/local-news/hawkesbury-ltc-outbreak-fuels-increase-in-eohu-covid-19-cases
[liii] Morgan, James. Prescott-Russell Residence COVID-19 case count remains at 48, four other outbreaks in effect across EOHU territory. The Review. October 20 2020. https://thereview.ca/2020/10/20/prescott-russell-residence-covid-19-case-count-remains-at-48-four-other-outbreaks-in-effect-across-eohu-territory/
[liv] Canadian Red Cross Supporting Long-Term Care Home in Hawkesbury. Ontario Newsroom. October 23 2020. https://news.ontario.ca/en/release/58920/canadian-red-cross-supporting-long-term-care-home-in-hawkesbury
[lv] Morgan, James. 38 residents remain positive for COVID-19 at Prescott and Russell Residence. The Review. October 28 2020. https://thereview.ca/2020/10/28/38-residents-remain-positive-for-covid-19-at-prescott-and-russell-residence/
[lvi] Morgan, James. Deaths due to COVID-19 at Prescott and Russell Residence reach 12, Hawkesbury business cases confirmed, town leads EOHU in active cases. The Review. November 2 2020. https://thereview.ca/2020/11/02/deaths-due-to-covid-19-at-prescott-and-russell-residence-reach-12-hawkesbury-business-cases-confirmed-town-leads-eohu-in-active-cases/
[lvii] Morgan, James. Prescott and Russell Residence COVID-19 outbreak results in 16 deaths, EOHU a yellow zone as of Saturday. The Review. November 6 2020. https://thereview.ca/2020/11/06/prescott-and-russell-residence-covid-19-outbreak-results-in-16-deaths-eohu-a-yellow-zone-as-of-saturday/
[lviii] Morgan, James. Eight new cases of COVID-19 at Prescott and Russell Residence. The Review. November 12 2020. https://thereview.ca/2020/11/12/eight-new-cases-of-covid-19-at-prescott-and-russell-residence/
[lix] Morgan, James. 29 cases of COVID-19 remain active at Prescott and Russell Residence, 141 active cases across EOHU territory. The Review. November 17 2020. https://thereview.ca/2020/11/17/29-cases-of-covid-19-remain-active-at-prescott-and-russell-residence-141-active-cases-across-eohu-territory/
[lx] Morgan, James. New COVID-19 cases at Prescott and Russell Residence, and an explanation of confusing case numbers. The Review. November 18 2020. https://thereview.ca/2020/11/18/new-covid-19-cases-at-prescott-and-russell-residence-and-an-explanation-of-confusing-case-numbers/
[lxi] Morgan, James. 106 active cases of COVID-19 across EOHU territory while Residence outbreak continues. The Review. November 24 2020. https://thereview.ca/2020/11/24/106-active-cases-of-covid-19-across-eohu-territory-while-residence-outbreak-continues/
[lxii] Morgan, James. One death, new cases of COVID-19 at Prescott and Russell Residence. The Review. November 25 2020. https://thereview.ca/2020/11/25/one-death-new-cases-of-covid-19-at-prescott-and-russell-residence/
[lxiii] Current cases in Halton. Halton Health Unit. November 26 2020. https://www.halton.ca/For-Residents/New-Coronavirus#01
[lxiv] Current cases in Halton. Halton Health Unit. November 19 2020. https://www.halton.ca/For-Residents/New-Coronavirus#01
[lxv] Long-Term Care Home COVID-19 Data. Government of Ontario. November 26 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[lxvi] Current cases in Halton. Halton Health Unit. November 26 2020. https://www.halton.ca/For-Residents/New-Coronavirus#01
[lxvii] Current cases in Halton. Halton Health Unit. November 30 2020. https://www.halton.ca/For-Residents/New-Coronavirus#01
[lxviii] Current cases in Halton. Halton Health Unit. October 14 2020. https://www.halton.ca/For-Residents/New-Coronavirus#01
[lxix] Mitchell, Don. Coronavirus: Hamilton reports 26 new COVID-19 cases, four new outbreaks. Global News. October 22 2020. https://globalnews.ca/news/7410681/coronavirus-hamilton-cases-oct-21/
[lxx] Current cases in Halton. Halton Health Unit. October 28 2020. https://www.halton.ca/For-Residents/New-Coronavirus#01
[lxxi] Mitchell, Don. Coronavirus: Hamilton reports just 2 COVID-19 cases as Ontario sets new daily record. Global News. November 4 2020. https://globalnews.ca/news/7438761/coronavirus-hamilton-cases-nov-3/
[lxxii] Mitchell, Don. Burlington, Oakville un-pause team sports, fitness classes amid new provincial COVID-19 framework. Global News. November 6 2020. https://globalnews.ca/news/7447003/burlington-oakville-sports-fitness-classes-resume-covid19/
[lxxiii] Long-Term Care Home COVID-19 Data. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[lxxiv] COVID-19 Update. Halton County Health Unit November 18 2020. https://www.halton.ca/For-Residents/Immunizations-Preventable-Disease/Diseases-Infections/New-Coronavirus/Status-of-COVID-19-Cases-in-Halton
[lxxv] COVID-19 Update. Halton County Health Unit November 26 2020. https://www.halton.ca/For-Residents/Immunizations-Preventable-Disease/Diseases-Infections/New-Coronavirus/Status-of-COVID-19-Cases-in-Halton
[lxxvi] Current cases in Halton. Halton Health Unit. November 30 2020. https://www.halton.ca/For-Residents/New-Coronavirus#01
[lxxvii] COVID-19 Update. Halton County Health Unit November 26 2020. https://www.halton.ca/For-Residents/Immunizations-Preventable-Disease/Diseases-Infections/New-Coronavirus/Status-of-COVID-19-Cases-in-Halton
[lxxviii] COVID-19 Update. Halton County Health Unit November 19 2020. https://www.halton.ca/For-Residents/Immunizations-Preventable-Disease/Diseases-Infections/New-Coronavirus/Status-of-COVID-19-Cases-in-Halton
[lxxix] COVID-19 Update. Halton County Health Unit November 26 2020. https://www.halton.ca/For-Residents/Immunizations-Preventable-Disease/Diseases-Infections/New-Coronavirus/Status-of-COVID-19-Cases-in-Halton
[lxxx] Current cases in Halton. Halton Health Unit. October 28 2020. https://www.halton.ca/For-Residents/New-Coronavirus#01
[lxxxi] Current cases in Halton. Halton Health Unit. November 9 2020. https://www.halton.ca/For-Residents/New-Coronavirus#01
[lxxxii] COVID-19 Update. Halton County Health Unit. November 17 2020. https://www.halton.ca/For-Residents/Immunizations-Preventable-Disease/Diseases-Infections/New-Coronavirus/Status-of-COVID-19-Cases-in-Halton
[lxxxiii] Mitchell, Don. Coronavirus: Hamilton reports 26 new COVID-19 cases, 3 deaths. Global News. November 24 2020. https://globalnews.ca/news/7481172/coronavirus-hamilton-cases-nov-24/
[lxxxiv] COVID-19 Update. Halton County Health Unit. November 26 2020. https://www.halton.ca/For-Residents/Immunizations-Preventable-Disease/Diseases-Infections/New-Coronavirus/Status-of-COVID-19-Cases-in-Halton
[lxxxv] Current cases in Halton. Halton Health Unit. November 30 2020. https://www.halton.ca/For-Residents/New-Coronavirus#01
[lxxxvi] COVID-19 Update. Hamilton Health Unit. November 17 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[lxxxvii] COVID-19 Update. Hamilton Health Unit. November 2 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[lxxxviii] COVID-19 Update. Hamilton Health Unit. November 18 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[lxxxix] Hristova, Bobby. Hamilton reports 74 new COVID-19 cases and 5 new deaths this weekend. CBC News. November 15 2020.
https://www.cbc.ca/news/canada/hamilton/hamilton-covid-19-1.5802874
[xc] COVID-19 Update. Hamilton Health Unit. November 17 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[xci] Hristova, Bobby. 112 new COVID-19 cases and 2 more deaths in Hamilton this weekend. CBC News. November 22 2020. https://www.cbc.ca/news/canada/hamilton/covid-19-hamilton-1.5811746
[xcii] COVID-19 Update. Hamilton Health Unit. November 26 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[xciii] COVID-19 Update. Hamilton Health Unit. November 27 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[xciv] Hristova, Bobby. 87 new COVID-19 cases in Hamilton, second record-breaking day in a row. CBC News. November 27 2020. https://www.cbc.ca/news/canada/hamilton/87-new-covid-19-cases-hamilton-1.5819687
[xcv] COVID-19 Update. Hamilton Health Unit. November 30 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[xcvi] COVID-19 Update. Hamilton Health Unit. November 30 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[xcvii] COVID-19 Update. Hamilton Health Unit. November 27 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[xcviii] COVID-19 Update. Hamilton Health Unit. November 30 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[xcix] Hristova, Bobby. Hamilton will enter full lockdown if COVID-19 cases keep rising: medical officer of health CBC News. November 30 2020. https://www.cbc.ca/news/canada/hamilton/monday-covid-19-cases-1.5821801
[c] Lorinc, Jacob. Four outbreaks reported in Hamilton over weekend, including one Sunday at long-term-care home. Hamilton Spectator. October 31 2020. https://www.thespec.com/news/hamilton-region/2020/10/31/covid-hamilton-latest-news-outbreaks.html?utm_source=facebook&source=the+hamilton+spectator&utm_medium=SocialMedia&utm_campaign=&utm_campaign_id=&utm_content
[ci] COVID-19 Update. Hamilton Health Unit. November 5 2020. https://www.hamilton.ca/coronavirus/status-cases
[cii] Mitchell, Don. Coronavirus: Hamilton reports 67 new COVID-19 cases, death at LTC. Global News. November 9 2020. https://globalnews.ca/news/7451781/coronavirus-hamilton-new-covid-19-cases-death-update-november-9/
[ciii] COVID-19 Update. Hamilton Health Unit. November 8 2020. https://www.hamilton.ca/coronavirus/status-cases
[civ] Hristova, Bobby. Hamilton reports 74 new COVID-19 cases and 5 new deaths this weekend. CBC News. November 15 2020.
https://www.cbc.ca/news/canada/hamilton/hamilton-covid-19-1.5802874
[cv] Mann, Ken. COVID-19 claims lives of two more long term care residents in Hamilton, public health says. 900 CHML. November 16 2020. https://globalnews.ca/news/7466027/covid-19-long-term-care-residents-hamilton/
[cvi] COVID-19 Update. Hamilton Health Unit. November 17 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[cvii] Hristova, Bobby. 112 new COVID-19 cases and 2 more deaths in Hamilton this weekend. CBC News. November 22 2020. https://www.cbc.ca/news/canada/hamilton/covid-19-hamilton-1.5811746
[cviii]Hristova, Bobby. Hamilton will enter full lockdown if COVID-19 cases keep rising: medical officer of health CBC News. November 30 2020. https://www.cbc.ca/news/canada/hamilton/monday-covid-19-cases-1.5821801
[cix] COVID-19 Update. Hamilton Health Unit. November 30 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[cx] A Bad Weekend for New Covid Cases in Ontario. The Bay Observer. November 9 2020. https://bayobserver.ca/2020/11/09/a-bad-weekend-for-new-covid-cases-in-ontario/
[cxi] COVID-19 Update. Hamilton Health Unit. November 8 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[cxii] Long-Term Care Home COVID-19 Data. Government of Ontario. November 18 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cxiii] Long-Term Care Home COVID-19 Data. Government of Ontario. November 22 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cxiv] Hristova, Bobby. 3 more deaths of people with COVID-19 in Hamilton on Tuesday. CBC News. November 24 2020. https://www.cbc.ca/news/canada/hamilton/covid-19-hamilton-1.5814055
[cxv] COVID-19 Update. Hamilton Health Unit. November 26 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[cxvi] COVID-19 Update. Hamilton Health Unit. November 30 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[cxvii] A Bad Weekend for New Covid Cases in Ontario. The Bay Observer. November 9 2020. https://bayobserver.ca/2020/11/09/a-bad-weekend-for-new-covid-cases-in-ontario/
[cxviii] Frketich, Joanna. Two more Hamilton seniors die as COVID spreads rapidly in long-term care homes. The Hamilton Spectator. November 10 2020. https://www.thespec.com/news/hamilton-region/2020/11/10/two-hamilton-seniors-die-as-covid-spreads-in-long-term-care-homes.html
[cxix] A Bad Weekend for New Covid Cases in Ontario. The Bay Observer. November 9 2020. https://bayobserver.ca/2020/11/09/a-bad-weekend-for-new-covid-cases-in-ontario/
[cxx] COVID-19 Update. Hamilton Health Unit. November 17 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[cxxi] COVID-19 Update. Hamilton Health Unit. November 20 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[cxxii] COVID-19 Update. Hamilton Health Unit. November 27 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[cxxiii] COVID-19 Update. Hamilton Health Unit. November 26 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[cxxiv] Mitchell, Don. Coronavirus: Hamilton reports 42 new COVID-19 cases, 3 deaths. Global News. November 23 2020. https://globalnews.ca/news/7479340/coronavirus-hamilton-cases-nov-23/
[cxxv] COVID-19 Update. Hamilton Health Unit. November 27 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[cxxvi] COVID-19 Update. Hamilton Health Unit. November 30 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton
[cxxvii] COVID-19 Update. Hamilton Health Unit. November 2 2020. https://www.hamilton.ca/coronavirus/status-cases
[cxxviii] Taekema, Dan. Chartwell says COVID-19 outbreak at Ancaster long-term care home has grown to 34 cases. CBC News. October 30 2020. https://www.cbc.ca/news/canada/hamilton/willowgrove-covid-outbreak-1.5783829
[cxxix] COVID-19 Update. Hamilton Health Unit. November 2 2020. https://www.hamilton.ca/coronavirus/status-cases
[cxxx] COVID-19 Update. Hamilton Health Unit. November 5 2020. https://www.hamilton.ca/coronavirus/status-cases
[cxxxi] McCullough, Kate. Outbreak declared at Dundas long-term-care home after 11 test positive; two new COVID-19 deaths in Hamilton. Hamilton Spectator. November 7 2020. https://www.thespec.com/news/hamilton-region/2020/11/07/covid-hamilton-outbreaks-latest-news.html?source=newsletter&utm_content=a02&utm_source=ml_nl&utm_medium=email&utm_email=D2560C0A4DECAFDAAD6AB9E4982348FC&utm_campaign=hshp_87300
[cxxxii] COVID-19 Update. Hamilton Health Unit. November 8 2020. https://www.hamilton.ca/coronavirus/status-cases
[cxxxiii] Mitchell, Don. Coronavirus: Hamilton reports 44 new COVID-19 cases, two more deaths. Global News. November 11 2020. https://globalnews.ca/news/7456312/coronavirus-hamilton-cases-nov-11/
[cxxxiv] Mitchell, Don. Coronavirus: Hamilton reports 46 new COVID-19 cases, 1 death at long-term care home. Global News. November 13 2020. https://globalnews.ca/news/7461444/coronavirus-hamilton-cases-nov-13/
[cxxxv] Frketich, Joanna. COVID cases are ‘exploding’ in long-term care and retirement homes. The Hamilton Spectator. November 17 2020. https://www.thespec.com/news/hamilton-region/2020/11/17/covid-cases-are-exploding-in-long-term-care-and-retirement-homes.html
[cxxxvi] Taekema, Dan. Public health orders nursing home where 14 residents have died to improve COVID-19 protections. CBC News. November 20 2020. https://www.cbc.ca/news/canada/hamilton/covid-willowgrove-1.5809920
[cxxxvii] Mitchell, Don. Coronavirus: Hamilton reports 26 new COVID-19 cases, 3 deaths. Global News. November 24 2020. https://globalnews.ca/news/7481172/coronavirus-hamilton-cases-nov-24/
[cxxxviii] COVID-19 Update. Hamilton Health Unit. November 27 2020. https://www.hamilton.ca/coronavirus/status-cases-in-hamilton. Note: the article says that there are cases in 4 visitors/others, but this is more than is reported by Hamilton Public Health on November 26, and the number has been changed accordingly.
[cxxxix] Benner, Allan. Another COVID-19 outbreak reported at regional nursing home. Niagara Falls Review. October 24 2020. https://www.niagarafallsreview.ca/news/niagara-region/2020/10/24/another-covid-19-outbreak-reported-at-regional-nursing-home.html
[cxl] Lafleche, Grant. Fort Erie long term care home site of biggest second wave COVID-19 outbreak in Niagara. St. Catharines Standard. November 3 2020. https://www.stcatharinesstandard.ca/news/niagara-region/2020/11/02/fort-erie-long-term-care-home-site-of-biggest-second-wave-covid-19-outbreak-in-niagara.html
[cxli] LaFleche, Grant. Six Gilmore Lodge residents with COVID-19 have died. St. Catharines Standard. November 6 2020. https://www.orangeville.com/news-story/10241248-six-gilmore-lodge-residents-with-covid-19-have-died/
[cxlii] Long-term care homes with an active outbreak. Government of Ontario. November 17 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cxliii] COVID-19 Update. Ottawa Health Unit November 17 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[cxliv] COVID-19 Update. Ottawa Health Unit November 17 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[cxlv] COVID-19 Update. Ottawa Health Unit November 17 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[cxlvi] COVID-19 Update. Ottawa Health Unit November 27 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[cxlvii] Daily COVID-19 Dashboard. Ottawa Public Health. October 28 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[cxlviii] Daily COVID-19 Dashboard. Ottawa Public Health. October 28 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[cxlix] Daily COVID-19 Dashboard. Ottawa Public Health. November 8 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[cl] COVID-19 Update. Ottawa Health Unit November 17 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[cli] COVID-19 Update. Ottawa Health Unit November 27 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[clii] Daily COVID-19 Dashboard. Ottawa Public Health. October 14 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[cliii] Daily COVID-19 Dashboard. Ottawa Public Health. November 11 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[cliv] COVID-19 Update. Ottawa Health Unit November 17 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[clv] COVID-19 Update. Ottawa Health Unit November 27 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[clvi] Daily COVID-19 Dashboard. Ottawa Public Health. October 28 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[clvii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[clviii] Daily COVID-19 Dashboard. Ottawa Public Health. November 8 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[clix] COVID-19 Update. Ottawa Health Unit November 17 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[clx] COVID-19 Update. Ottawa Health Unit November 27 2020. https://www.ottawapublichealth.ca/en/reports-research-and-statistics/daily-covid19-dashboard.aspx
[clxi] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 27 2020. https://peelregion.ca/coronavirus/case-status/
[clxii] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 13 2020. https://peelregion.ca/coronavirus/case-status/
[clxiii] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 24 2020. https://peelregion.ca/coronavirus/case-status/
[clxiv] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 27 2020. https://peelregion.ca/coronavirus/case-status/
[clxv] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 27 2020. https://peelregion.ca/coronavirus/case-status/
[clxvi] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 24 2020. https://peelregion.ca/coronavirus/case-status/
[clxvii] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 27 2020. https://peelregion.ca/coronavirus/case-status/
[clxviii] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. December 1 2020. https://peelregion.ca/coronavirus/case-status/
[clxix] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 27 2020. https://peelregion.ca/coronavirus/case-status/
[clxx] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 13 2020. https://peelregion.ca/coronavirus/case-status/
[clxxi] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 24 2020. https://peelregion.ca/coronavirus/case-status/
[clxxii] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 27 2020. https://peelregion.ca/coronavirus/case-status/
[clxxiii] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. December 1 2020. https://peelregion.ca/coronavirus/case-status/
[clxxiv] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 27 2020. https://peelregion.ca/coronavirus/case-status/
[clxxv] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 13 2020. https://peelregion.ca/coronavirus/case-status/
[clxxvi] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 24 2020. https://peelregion.ca/coronavirus/case-status/
[clxxvii] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. November 27 2020. https://peelregion.ca/coronavirus/case-status/
[clxxviii] Long-Term Care and Retirement Home Outbreaks in Peel. Peel Region. December 1 2020. https://peelregion.ca/coronavirus/case-status/
[clxxix] Active Institutional Outbreak Information. Thunder Bay District Health Unit. December 1 2020. https://www.tbdhu.com/coviddata
[clxxx] Rinne, Gary. UPDATED: COVID-19 outbreak declared at Southbridge Roseview nursing home. Tbnewswatch.com. November 18 2020. https://www.tbnewswatch.com/local-news/covid-19-outbreak-declared-at-southbridge-roseview-nursing-home-2888424
[clxxxi] Diaczuk, Doug. Paramedics provide COVID-19 testing to Roseview Manor staff amid outbreak. Tbnewswatch.com. November 26 2020. https://www.tbnewswatch.com/local-news/paramedics-provide-covid-19-testing-to-roseview-manor-staff-amid-outbreak-3130971
[clxxxii] Second Roseview resident passes away from COVID-19. Tbnewswatch.com. November 30 2020. https://www.tbnewswatch.com/local-news/second-roseview-resident-passes-away-from-covid-19-3138289
[clxxxiii] Outbreaks in Toronto Healthcare Institutions. City of Toronto. October 28 2020. https://open.toronto.ca/dataset/outbreaks-in-toronto-healthcare-institutions/
[clxxxiv] Long-Term Care Home COVID-19 Data. Government of Ontario. October 28 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[clxxxv] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[clxxxvi] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[clxxxvii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[clxxxviii] Long-term care homes with an active outbreak. Government of Ontario. November 9 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[clxxxix] Long-term care homes with an active outbreak. Government of Ontario. November 16 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cxc] Long-term care homes with an active outbreak. Government of Ontario. November 16 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cxci] Long-term care homes with an active outbreak. Government of Ontario. November 16 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cxcii] Active Outbreaks. Government of Ontario. November 30 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cxciii] Active Outbreaks. Government of Ontario. November 30 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cxciv] COVID-19 Updates. Southbridge Care Homes. December 1 2020. https://www.southbridgecarehomes.com/covid-19-updates
[cxcv] Active Outbreaks. Government of Ontario. December 2 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cxcvi] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cxcvii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cxcviii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cxcix] Long-term care homes with an active outbreak. Government of Ontario. November 9 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cc] Active Outbreaks. Government of Ontario. November 30 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cci] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccii] Wednesday, September 16 – 3 pm. Organizational Update. Schlegel Villages. September 16 2020. https://schlegelvillages.com/sites/default/files/website_files/sept_16_daily_update_poster.docx
[cciii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cciv] Jabakhanji, Sara. Toronto long-term care home grappling with outbreak reports 42 active COVID-19 cases, including 1 death. Toronto CBC News. September 29 2020. https://www.cbc.ca/news/canada/toronto/fairview-nursing-home-outbreak-covid19-1.5743503
[ccv] Long-Term Care Home COVID-19 Data. Government of Ontario. October 15 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccvi] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccvii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccviii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccix] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccx] Outbreaks in Toronto Healthcare Institutions. City of Toronto. November 30 2020. https://open.toronto.ca/dataset/outbreaks-in-toronto-healthcare-institutions/
[ccxi] Long-Term Care Home COVID-19 Data. Government of Ontario. November 17 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxii] Long-Term Care Home COVID-19 Data. Government of Ontario. November 17 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxiii] COVID-19 Reports. Sienna Senior Living. November 30 2020. https://www.siennaliving.ca/covid-19-updates
[ccxiv] Outbreaks in Toronto Healthcare Institutions. City of Toronto. October 28 2020. https://open.toronto.ca/dataset/outbreaks-in-toronto-healthcare-institutions/
[ccxv] Long-Term Care Home COVID-19 Data. Government of Ontario. October 28 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxvi] Long-Term Care Home COVID-19 Data. Government of Ontario. October 28 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxvii] Long-Term Care Home COVID-19 Data. Government of Ontario. October 28 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxviii] Long-Term Care Home COVID-19 Data. Government of Ontario. Nov 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxix] Long-term care homes with an active outbreak. Government of Ontario. November 16 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[ccxx] Long-term care homes with an active outbreak. Government of Ontario. November 16 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[ccxxi] Gowans, Sue. Twitter. November 15 2020. https://twitter.com/Sue_Innovates/status/1328002888401100801
[ccxxii] Fox, Chris. Nearly half of all residents at city-run long-term care home downtown have tested positive for COVID-19. CP24. November 18 2020. https://www.cp24.com/news/nearly-half-of-all-residents-at-city-run-long-term-care-home-downtown-have-tested-positive-for-covid-19-1.5194688
[ccxxiii] Levy, Sue-Ann. Massive outbreak at city-operated LTC. Toronto Sun. November 18 2020. https://torontosun.com/news/local-news/massive-outbreak-at-city-operated-ltc
[ccxxiv] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxxv] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxxvi] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxxvii] COVID-19 Reports : Care Communities and Retirement Residences. Sienna Living. November 9 2020. https://www.siennaliving.ca/covid-19-updates
[ccxxviii] Long-term care homes with an active outbreak. Government of Ontario. November 16 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[ccxxix] Long-term care homes with an active outbreak. Government of Ontario. November 16 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[ccxxx] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxxxi] COVID-19 Reports. Sienna Senior Living. November 30 2020. https://www.siennaliving.ca/covid-19-updates
[ccxxxii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxxxiii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxxxiv] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxxxv] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxxxvi] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxxxvii] Media Statement – Outbreak at Kennedy Lodge Long Term Care Home – Scarborough. Revera. October 26 2020. https://cdn.reveraliving.com/-/media/files/covid-19/oct-2020/media-statement-kennedy-lodge-scarborough-ltc-oct-26-2020.pdf?rev=2cba4c5fd76d4fc39c3eee623528f15d&hash=3E206E5C043E41726F2BC4EEAA6839A6&_ga=2.175290661.625373901.1604323814-2022651287.1604323814
[ccxxxviii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxxxix] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxl] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxli] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxlii] 29 residents of Toronto long-term care home dead after COVID-19 outbreak. The Canadian Press. November 11 2020. https://nationalpost.com/news/canada/twenty-nine-residents-of-toronto-long-term-care-home-died-in-latest-covid-19-outbreak
[ccxliii] Media Statement – Update on Kennedy Lodge Long Term Care Home – Scarborough. Revera. November 13 2020. https://cdn.reveraliving.com/-/media/files/covid-19/nov-2020/media-statement-kennedy-lodge-scarborough-ltc-nov13-2020.pdf?rev=90ab6c0c9adb4c8396ca697f0976b8d2&hash=D2171C3361C1A672195E679C8858BF73&_ga=2.20779448.1230650195.1605554266-315566138.1605122177
[ccxliv] Media Statement – Update on Kennedy Lodge Long Term Care Home – Scarborough. Revera. November 26 2020. https://cdn.reveraliving.com/-/media/files/covid-19/nov-2020/media-statement-kennedy-lodge-scarborough-ltc-nov26-2020.pdf?rev=31cf7f92dacb48d6b4130072590f6c2b&hash=D63DF169E808394BE5D0AC321CC59C9A&_ga=2.77112341.1263506044.1606760780-2022651287.1604323814
[ccxlv] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxlvi] Active Outbreaks. Government of Ontario. October 15 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data/resource/4b64488a-0523-4ebb-811a-fac2f07e6d59
[ccxlvii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxlviii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxlix] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccl] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccli] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclii] Long-term care homes with an active outbreak. Government of Ontario. November 16 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[ccliii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccliv] Media Statement – COVID-19 outbreak at Main Street Terrace Long Term Care Home –Toronto. Revera. October 23 2020. https://cdn.reveraliving.com/-/media/files/covid-19/oct-2020/media-statement-mainstreetterrace-toronto-ltc-oct23-2020.pdf?rev=bfb724c2fbbe451aa1972d19e7cda2a9&hash=CA98CACF9B5DFDF31C6C587BB7C079B7&_ga=2.120164623.625373901.1604323814-2022651287.1604323814
[cclv] Long-Term Care Home COVID-19 Data. Government of Ontario. October 28 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclvi] Raza, Ali. Main Street Terrace long-term care home reporting 56 cases of COVID-19 among residents. Beach Metro Community News. October 30 2020. https://www.beachmetro.com/2020/10/30/main-street-terrace-long-term-care-home-reporting-56-cases-of-covid-19-among-residents/?fbclid=IwAR2D4t0-p-3i6cheKB-zId35ZcO8Y636KEEfYh5XdsNHSY63PEmk03_bfVA
[cclvii] Crawford, Blair. Ottawa’s Extendicare Starwood COVID-19 outbreak the worst in the province. Ottawa Citizen. November 3 2020. https://ottawacitizen.com/news/local-news/ottawas-extendicare-starwood-covid-19-outbreak-the-worst-in-the-province
[cclviii] Crawford, Blair. Ottawa’s Extendicare Starwood COVID-19 outbreak the worst in the province. Ottawa Citizen. November 3 2020. https://ottawacitizen.com/news/local-news/ottawas-extendicare-starwood-covid-19-outbreak-the-worst-in-the-province
[cclix] Aguilar, Bryann. 29 residents dead from COVID-19 at Scarborough long-term care home. CP24. November 11 2020. https://toronto.ctvnews.ca/29-residents-dead-from-covid-19-at-scarborough-long-term-care-home-1.5185186
[cclx] Media Statement – Update on Main Street Terrace Long Term Care Home – Toronto. Revera. November 24 2020. https://cdn.reveraliving.com/-/media/files/covid-19/nov-2020/media-statement-main-street-terrace-toronto-ltc-nov24-2020.pdf?rev=b103749055e2440faec7e99ba19bf21b&hash=8724ADB04100D8B863090CD70D3E1A82&_ga=2.73582354.1263506044.1606760780-2022651287.1604323814
[cclxi] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxiii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxiv] Long-term care homes with an active outbreak. Government of Ontario. November 9 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cclxv] Long-term care homes with an active outbreak. Government of Ontario. November 16 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cclxvi] Long-term care homes with an active outbreak. Government of Ontario. November 16 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cclxvii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxviii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxix] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxx] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxxi] COVID-19 Reports : Care Communities and Retirement Residences. Sienna Living. November 9 2020. https://www.siennaliving.ca/covid-19-updates
[cclxxii] Long-term care homes with an active outbreak. Government of Ontario. November 16 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cclxxiii] Elpa, Ann Marie. Eight residents dead at Scarborough care home in COVID-19 outbreak. Toronto Star. November 14 2020. https://www.thestar.com/news/gta/2020/11/14/seven-residents-dead-at-scarborough-care-home-in-covid-19-outbreak.html
[cclxxiv] Active Outbreaks. Government of Ontario. November 30 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxxv] Active Outbreaks. Government of Ontario. November 30 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxxvi] COVID-19 Reports. Sienna Senior Living. November 30 2020. https://www.siennaliving.ca/covid-19-updates
[cclxxvii] Long-Term Care Home COVID-19 Data. Government of Ontario. October 15 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxxviii] Long-Term Care Home COVID-19 Data. Government of Ontario. November 17 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxxix] Long-Term Care Home COVID-19 Data. Government of Ontario. November 17 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxxx] Active Outbreaks. Government of Ontario. November 30 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxxxi] Outbreaks in Toronto Healthcare Institutions. City of Toronto. November 30 2020. https://open.toronto.ca/dataset/outbreaks-in-toronto-healthcare-institutions/
[cclxxxii] Active Outbreaks. Government of Ontario. November 20 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxxxiii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxxxiv] Long-Term Care Home COVID-19 Data. Government of Ontario. October 15 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxxxv] Long-term care home closed to visitors amid COVID-19 outbreak in Toronto. Toronto CBC News. October 3 2020. https://www.cbc.ca/news/canada/toronto/vermont-square-long-term-care-home-covid-10-outbreak-1.5749483
[cclxxxvi] Long-term care homes with an active outbreak. Government of Ontario. October 14 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19#13
[cclxxxvii] Aguilar, Bryann. Nearly half of residents at long-term care home near The Annex have tested positive for COVID-19. CP24. October 25 2020.
https://www.cp24.com/mobile/news/nearly-half-of-residents-at-long-term-care-home-near-the-annex-have-tested-positive-for-covid-191.5160369?cid=sm%3Atrueanthem%3Acp24%3Apost&utm_campaign=trueAnthem%3A%20Trending%20Content&utm_medium=trueAnthem&utm_source=facebook&fbclid=IwAR2CA98yeBrZLs_IjBMLHmZRrbxxx-tFeqje-acwMyQMOwdMB8899o-cuGc
[cclxxxviii] Active Outbreaks. Government of Ontario. November 9 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cclxxxix] Active Outbreaks. Government of Ontario. November 20 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxc] Outbreaks in Toronto Healthcare Institutions. City of Toronto. November 30 2020. https://open.toronto.ca/dataset/outbreaks-in-toronto-healthcare-institutions/
[ccxci] Media Statement – COVID-19 Outbreak at Westside Long Term Care Home – Toronto. Revera. November 14 2020. https://cdn.reveraliving.com/-/media/files/covid-19/nov-2020/media-statement-westside-toronto-ltc-nov14-2020-rev.pdf?rev=303af06467c745dba0018198f0a1fbbf&hash=D7107F52439437562CB321F6D00C04EA&_ga=2.187433768.1263506044.1606760780-2022651287.1604323814
[ccxcii] Media Statement – COVID-19 Outbreak at Westside Long Term Care Home – Toronto. Revera. November 14 2020. https://cdn.reveraliving.com/-/media/files/covid-19/nov-2020/media-statement-westside-toronto-ltc-nov14-2020-rev.pdf?rev=303af06467c745dba0018198f0a1fbbf&hash=D7107F52439437562CB321F6D00C04EA&_ga=2.187433768.1263506044.1606760780-2022651287.1604323814
[ccxciii] Media Statement – COVID-19 Outbreak at Westside Long Term Care Home – Toronto. Revera. November 15 2020. https://cdn.reveraliving.com/-/media/files/covid-19/nov-2020/media-statement-westside-toronto-ltc-nov15-2020-rev.pdf?rev=9edafd6929e3495dab3e32e78bd01cc3&hash=E5982ED3B864F7C6C82125E6C658FD35&_ga=2.178825252.1263506044.1606760780-2022651287.1604323814
[ccxciv] Active Outbreaks. Government of Ontario. November 20 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[ccxcv] Media Statement – Update on outbreak at Westside Long Term Care Home – Toronto. Revera. November 26 2020. https://cdn.reveraliving.com/-/media/files/covid-19/nov-2020/media-statement-westside-toronto-ltc-nov26-2020.pdf?rev=c1f523f8377744cca40a5202204df7aa&hash=789D2047922C101C6EA6EA536CE87116&_ga=2.81766423.1263506044.1606760780-2022651287.1604323814
[ccxcvi] Media Statement – Update on outbreak at Westside Long Term Care Home – Toronto. Revera. November 30 2020. https://cdn.reveraliving.com/-/media/files/covid-19/nov-2020/media-statement-westside-toronto-ltc-nov30-2020.pdf?rev=ee285c1a8f8544a786b73e16038f6871&hash=8A25D41F3AA3300FCB20336DAC448F98&_ga=2.229228060.1415421515.1606919145-2022651287.1604323814
[ccxcvii] Long-term care resident and family face concerns as COVID outbreak spikes to 15 cases at Iler Lodge. CBC News. November 12 2020. https://www.cbc.ca/news/canada/windsor/iler-lodge-ltc-covid-15-cases-1.5800255
[ccxcviii] Local COVID-19 Data. Windsor Essex Public Health. November 9 2020. https://www.wechu.org/cv/local-updates
[ccxcix] Long-term care resident and family face concerns as COVID outbreak spikes to 15 cases at Iler Lodge. CBC News. November 12 2020. https://www.cbc.ca/news/canada/windsor/iler-lodge-ltc-covid-15-cases-1.5800255
[ccc] Local COVID-19 Data. Windsor Essex Public Health. November 17 2020. https://www.wechu.org/cv/local-updates
[ccci] Local COVID-19 Data. Windsor Essex Public Health. November 27 2020. https://www.wechu.org/cv/local-updates
[cccii] Local COVID-19 Data. Windsor Essex Public Health. November 27 2020. https://www.wechu.org/cv/local-updates
[ccciii] https://windsor.ctvnews.ca/38-new-covid-19-cases-in-windsor-essex-one-new-potential-public-exposure-at-leamington-church-wechu-1.5199183
[ccciv] Local COVID-19 Data. Windsor Essex Public Health. November 27 2020. https://www.wechu.org/cv/local-updates
[cccv] Zarzour, Kim. UPDATED: ‘A horrible situation for everyone’: Vaughan long-term care home 1 of several Ontario facilities battling surge of COVID-19. Vaughan Citizen. October 29 2020. https://www.yorkregion.com/news-story/10232928–a-horrible-situation-for-everyone-vaughan-long-term-care-home-1-of-several-ontario-facilities-battling-surge-of-covid-19/?fbclid=IwAR0Modix_I8XC2hVApA3PKlWjsGZYDt_1aXQahh_aAXGluToEDIKZUVACWU
[cccvi] Zarzour, Kim. UPDATED: ‘A horrible situation for everyone’: Vaughan long-term care home 1 of several Ontario facilities battling surge of COVID-19. Vaughan Citizen. October 29 2020. https://www.yorkregion.com/news-story/10232928–a-horrible-situation-for-everyone-vaughan-long-term-care-home-1-of-several-ontario-facilities-battling-surge-of-covid-19/?fbclid=IwAR0Modix_I8XC2hVApA3PKlWjsGZYDt_1aXQahh_aAXGluToEDIKZUVACWU
[cccvii] Long-term care homes with an active outbreak. Government of Ontario. November 9 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cccviii] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 9 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s
[cccix] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 13 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s
[cccx] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 17 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s
[cccxi] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 27 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s
[cccxii] Long-term care homes with an active outbreak. Government of Ontario. November 9 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cccxiii] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 13 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s
[cccxiv] Kelly, Debora. COVID-19 Today: A look at the numbers for Newmarket, York Region, Ontario. Newmarket Today. November 21 2020. https://www.newmarkettoday.ca/coronavirus-covid-19-local-news/covid-19-today-a-look-at-the-numbers-for-newmarket-york-region-ontario-2898729
[cccxv] Active Outbreaks. Government of Ontario. November 27 2020. https://data.ontario.ca/dataset/long-term-care-home-covid-19-data
[cccxvi] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 27 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s
[cccxvii] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 30 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s
[cccxviii] Long-term care homes with an active outbreak. Government of Ontario. November 13 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cccxix] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 13 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s
[cccxx] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 27 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s
[cccxxi] Long-term care homes with an active outbreak. Government of Ontario. November 9 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cccxxii] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 13 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s
[cccxxiii] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 27 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s
[cccxxiv] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 30 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s
[cccxxv] Long-term care homes with an active outbreak. Government of Ontario. November 9 2020. https://www.ontario.ca/page/how-ontario-is-responding-covid-19
[cccxxvi] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 27 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s
[cccxxvii] Outbreaks in Long-Term Care and Community Settings. The Regional Municipality of York. November 30 2020. https://www.york.ca/wps/portal/yorkhome/!ut/p/z1/04_Sj9CPykssy0xPLMnMz0vMAfIjo8zijYxMzDwMnQ28DDz8LQw83cwDTF0sPAwNvI30wwkpiAJKG-AAjgZA_VGElBTkRhikOyoqAgC__eMj/dz/d5/L2dBISEvZ0FBIS9nQSEh/#.XsYQ6hNKh0s